

When you or your partner is living with chronic pain from a rheumatic or musculoskeletal condition like arthritis — that often come along with other issues like brain fog, fatigue, or depression and anxiety, to name a few common ones — your sex life can change, sometimes dramatically.
But when even talking about these concerns with your partner seems formidable, it’s hard to imagine being able to do something about it to make things better.
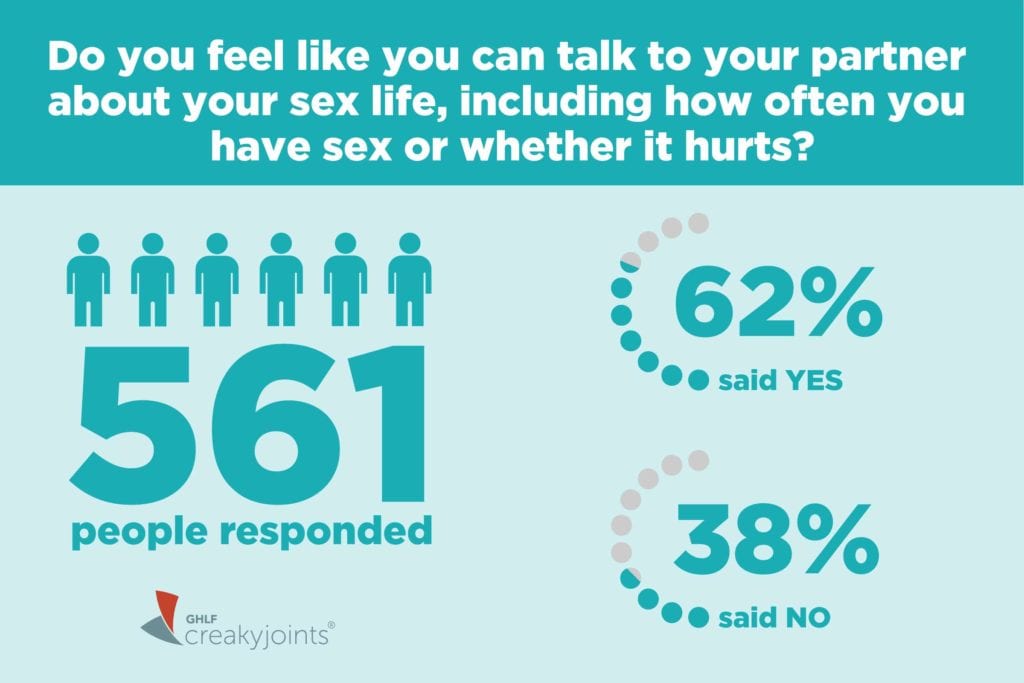
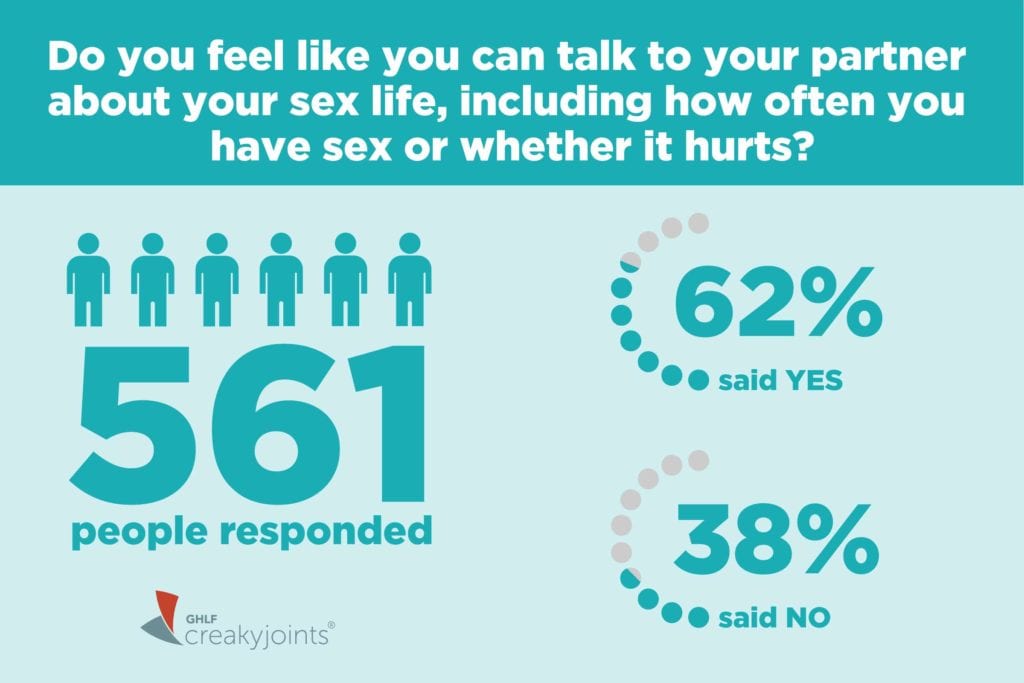
In a recent ArthritisPower community poll, we asked whether people feel like theycan talk to their partner about their sex life, including how often they have sex or whether it hurts? Out of 561 respondents, 62 percent said that yes, they did feel like they could talk to their partners about their sex lives — and that’s great news.
But for the 38 percent of respondents who didn’t feel that way, or even for those among the majority who could use advice on how to make those conversations more productive or supportive, we talked to a psychologist and a rheumatologist for their perspectives.
Sexual Health and Arthritis: Understanding the Issues
First, it’s important to realize how common sexual health issues are for people with arthritis. “Most people with arthritis pain will experience some kind of sexual dysfunction,” says Kim Gorgens, PhD,clinical professor and director of continuing education at the Graduate School of Professional Psychology at the University of Denver. “That means that pain is the norm, not the exception.” In fact, a new study in the Journal of Rheumatology found that 48 percent of women with rheumatoid arthritis experienced sexual dysfunction. As a comparison, only 14 percent of healthy women in a control group reported sexual dysfunction.
Even simply being aware of how common sexual health concerns are for people with arthritis or chronic pain is critically important, says Dr. Gorgens.
In her community clinics, a sign that reads “Sex is spoken here” hangs prominently so patients can see it. The message they’re looking to convey: “Your sexual health is just as important as your physical health,” says Dr. Gorgens. “This is the hardest part for folks: Recognizing that they need to prioritize their sexual health, that it matters as much as anything else they’re coping with.”
The Types of Sexual Dysfunction
Sexual dysfunction falls into three general categories, medically speaking, according to Dr. Gorgens. They’re all inter-related to each other, and it’s important for people with chronic pain to understand all three and how these issues might affect them or their partners.
- Primary sexual dysfunction refers to impaired libido, poor lubrication, inability to orgasm.
- Secondary sexual dysfunction refers to physical limitations, such as joint pain or limited mobility, that can affect your ability to engage in or enjoy sexual activity
- Tertiary sexual dysfunction refers to psychological or emotional issues related to how you think about your sex life. For example, this could include feeling shameful about having sexual needs, or guilt over feeling like you have to suppress your sexual self because of pain.
How to Talk About Sex and Arthritis
Dr. Gorgens describes a strategy she calls the three Rs: recognize, rapport, and research. “Having this simple framework takes some of the mystery and ambiguity out of the conversation,” she says.
Recognize means first understanding the need to prioritize your sexual health. Be reflective and identify the issues that you’re concerned about or that you suspect your partner is concerned about.
This could include how often you engage in sex with your partner — and if there’s an unmet need for either of you, how sex feels physically and emotionally, and how different aspects of your disease are affecting your sexual health. It’s important to first do this reflecting, says Dr. Gorgens, so you can know exactly what to broach with your care provider or partner.
Rapport means establishing the support you need to start thinking about solutions for your sexual health concerns. At your provider’s office, this could mean sharing frustrations or issues with your nurse or doctor the same way you would if you were having issues with other aspects of daily living.
“In general, physicians don’t do a great job bringing up sexual health during routine discussions,” says Erin Bauer, MD, a rheumatologist at Virginia Mason Medical Center in Seattle, Washington. “But every provider would want to know if your disease is affecting your sexual health, even if we don’t bring it up first.”
She points out that if there are issues related to a medication’s side effects, your doctor can help you explore other options. If there are issues related to physical limitations or discomfort, your doctor can help you see a physical or occupational therapist.
Rapport also includes the importance of seeking support from the arthritis community at large: finding other patients who are going through the same things you are and who can listen and share advice.
With your partner, rapport means sharing your concerns with each other. “You can assume everyone’s stumbled through this conversation or attempting to have this conversation,” says Dr. Gorgens. “There’s no perfect way to do it, but you just have to try. One partner might feel offended or not heard, but that’s where ‘research’ comes in.”
Research means looking for ways to make things better, both in terms of communication with your partner or provider and in terms of identifying tips and strategies to improve your sexual health.
This could include things like switching to a medication that doesn’t make you feel as nauseous, using moist heat or taking pain medication before sex to help with pain control, experimenting with self-pleasure, and more.
“There’s a way around every barrier and the right providers will help you,” says Dr. Gorgens. “The universe of assistive aids grows by the minute.”





