Have you ever heard of calcium pyrophosphate (CPP)? Unless you’re having a specific type of joint pain, we’re guessing not.
Calcium pyrophosphate is a normal chemical in the body that helps your bones and joints function.
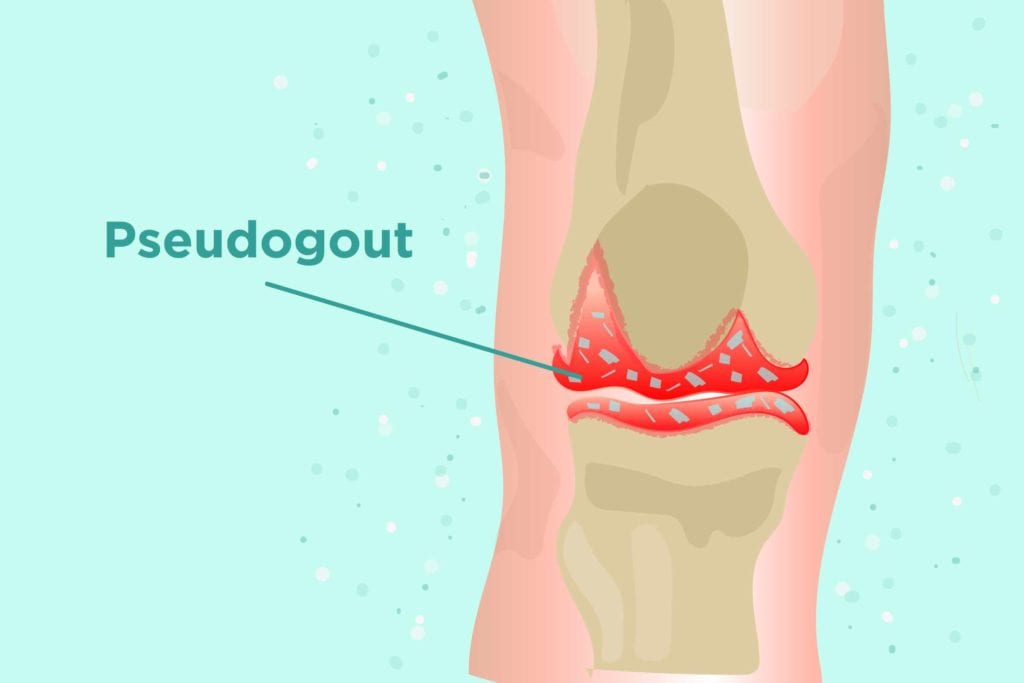
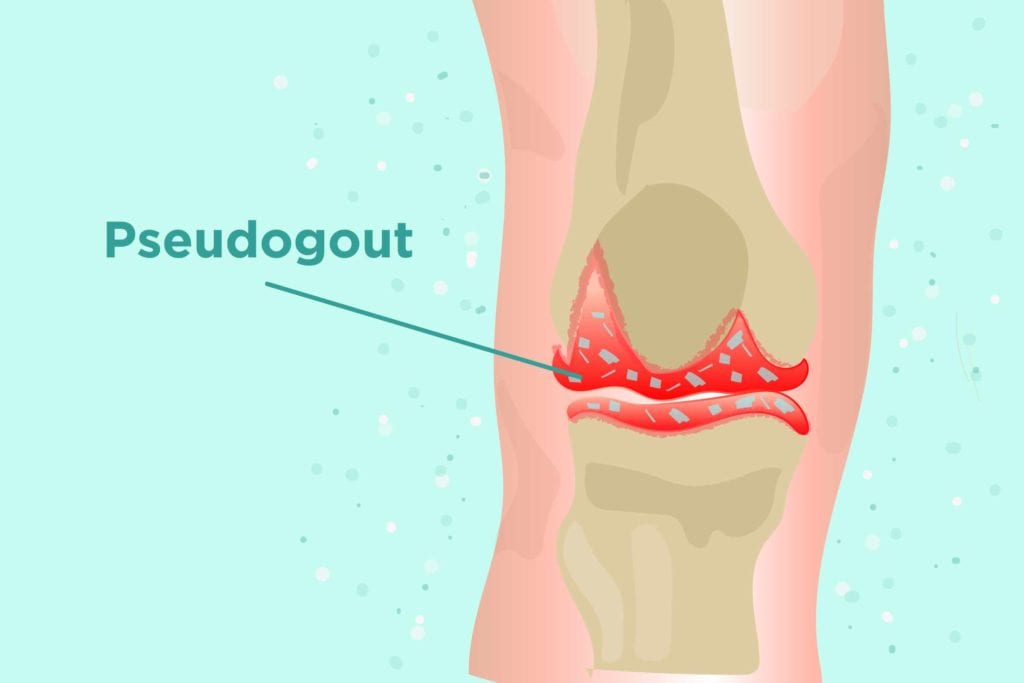
But in some people, the substance builds up into crystals in the cartilage, the connective tissue in your joints, over time and with age. As those crystals accumulate and make their way into the joint fluid, they can irritate or damage the joints, leading to an arthritis known by different names: calcium pyrophosphate dihydrate deposition disease (CPPD), acute CPP crystal arthritis, or pseudogout.
Pseudogout vs. Gout
As its name suggests, pseudogout has some similarities with gout. Both types of arthritis are caused by buildups of crystals — CPP for pseudogout and uric acid for gout — though the two look different, says Graham Hughes, MD, consultant rheumatologist and head of the London Lupus Centre with HCA Healthcare UK.
“Regular gout is needle-shaped crystals in the joints,” he says. “Pseudogout is these rhomboid-shaped crystals — four sides but leaning.” The joints affected by each condition also tend to be different, with pain and swelling in the big toe being the classic symptom of regular gout. Pseudogout is more likely to strike the knee or wrist.
Pseudogout vs. Other Arthritis
Pseudogout can also mimic other types of arthritis, including osteoarthritis. Both get more common with age, and there’s overlap in the affected joints. In fact, some evidence suggests that having pseudogout can lead to or worsen osteoarthritis, with the CPP crystals contributing to wear and tear of the joints.
Pseudogout is also sometimes misdiagnosed as rheumatoid arthritis (RA). Those patients will likely have high levels of inflammatory markers but will test negative for RA-associated antibodies rheumatoid factor and anti-cyclic citrullinated peptide, says John Davis III, MD, a rheumatologist with the Mayo Clinic
What Are the Symptoms of Pseudogout?
Pseudogout symptoms aren’t constant; they tend to come and go. During a flare, though, the joints can become painful, swollen, and inflamed.
“It affects joints that are typically not affected in garden-variety osteoarthritis,” says Dr. Davis. Most commonly, pseudogout appears in the knees and sometimes the wrist, though it can also affect the hips, ankles, and other joints. In most cases, pseudogout will only affect one or two joints.
Causes of Pseudogout
Researchers aren’t sure exactly what makes CPP crystals build up in the joints and cause pain, but there are some risk factors involved. By age 90, about half of people will have CPP crystals in the joints, though they won’t necessarily show symptoms.
In some people, there seems to be a genetic component that predisposes them to higher pyrophosphate levels, which in turn sets them up for excess CPP crystals.
Other mineral imbalances can also be risk factors, with conditions causing high calcium (hyperparathyroidism), excess iron (hemochromatosis), and low magnesium (hypomagnesemia) also contributing to the CPP crystal build-up, says Dr. Davis. The risk increases with age, and also after injury or surgery.
How Doctors Diagnose Pseudogout
If you’re experiencing symptoms you and your doctor think could be pseudogout, your doctor might start by ordering blood tests like sedimentation rate or C-reactive protein, which measure inflammation in the body. Those will be higher in a person with inflammatory arthritis like pseudogout, but they aren’t specific, which means they could point toward a whole slew of inflammatory conditions, like rheumatoid arthritis and lupus.
What really clinches a pseudogout diagnosis is a sign straight from the joints. “Ideally you’re trying to find evidence of the crystal deposition,” says Dr. Davis. A doctor can take synovial fluid — a thick liquid that helps joints move smoothly — from the affected area and check it for those diamond-shaped crystals.
Less commonly, X-rays can also show signs of pseudogout. The imaging can reveal calcification in the knee or wrist, which suggests pseudogout, says Dr. Hughes.
How Pseudogout Is Treated
Although there’s no cure for pseudogout, there are effective therapies that prevent flares. Nonsteroidal anti-inflammatory drugs (NSAIDs) can be a first line of treatment for pain, but pseudogout patients might need to take extra measures to keep the disease in check. Rheumatologists sometimes prescribe colchicine, an anti-inflammatory gout medication that can prevent flares, though it isn’t effective for short-term relief, says Dr. Davis.
Other pseudogout patients might find relief from corticosteroids such as prednisone, either as an injection or an oral medication prescription. The steroids reduce inflammation but can cause serious complications if used long-term.
In some cases, the doctor might drain the joint fluid to help get rid of some of the crystals before injecting the corticosteroid. “It’s very dramatically successful,” says Dr. Hughes. “If you’re lucky, that does it overnight. The patient is better, and the pain is almost gone.”
Keep Reading
- Gout vs. Rheumatoid Arthritis: What’s the Difference?
- NSAIDs Can Wreck Your Stomach If You’re Not Careful: Are You at Risk?
- Common Questions About Taking Prednisone





