Is a 0-10 Pain Scale Really the Best Way to Convey Your Pain?
That’s the question we posed in our July 2018 monthly poll to participants in ArthritisPower®, our patient-centered research registry for joint, bone, and inflammatory skin conditions.
More than half of poll respondents (59 percent) thought that using a numbering system was not an effective method to measure their pain.
This echoes a change in thinking among some in the medical community, who say that these pain scales are too simplistic and could lead to patients not getting the most effective treatment for their pain.
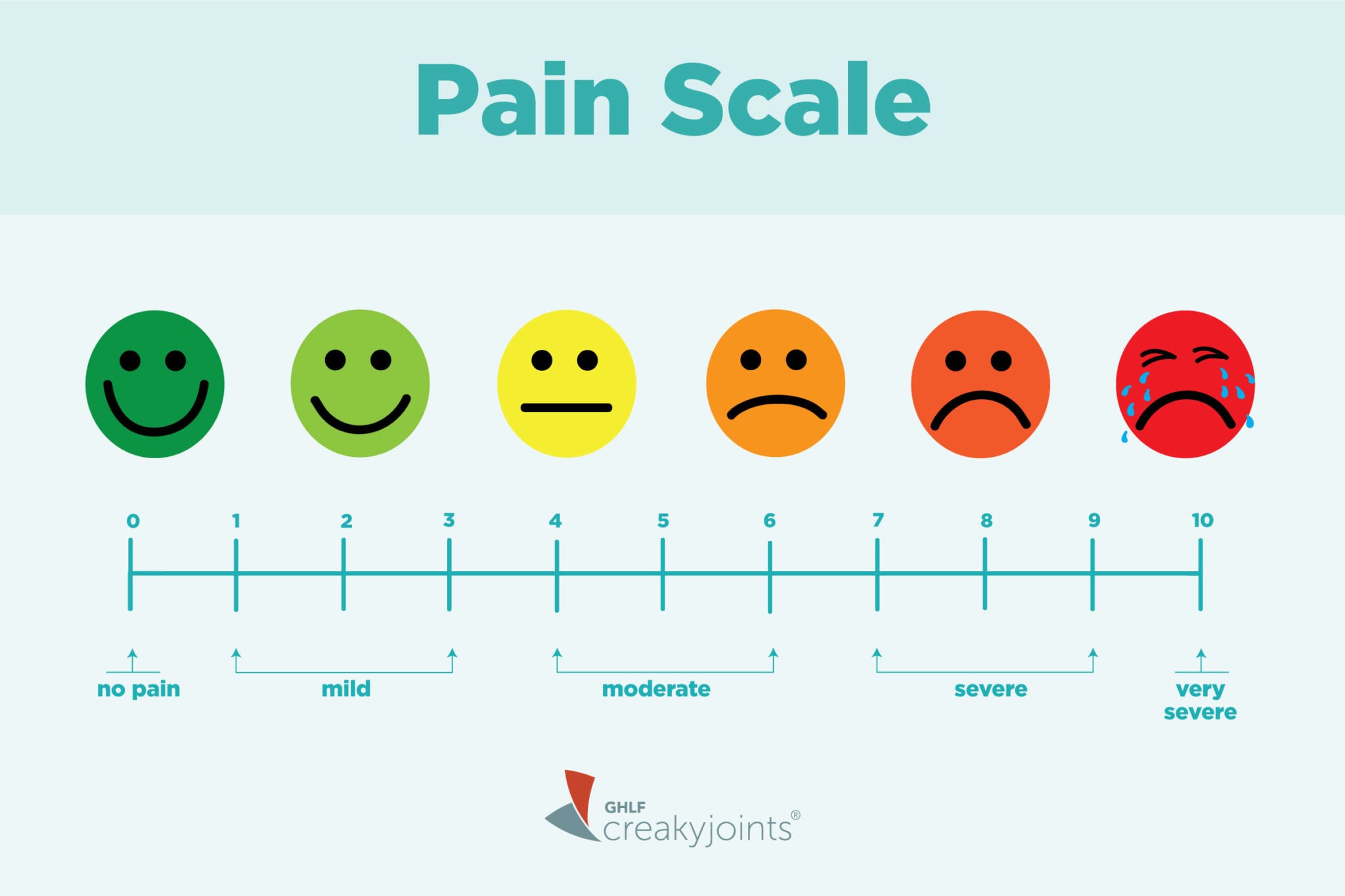
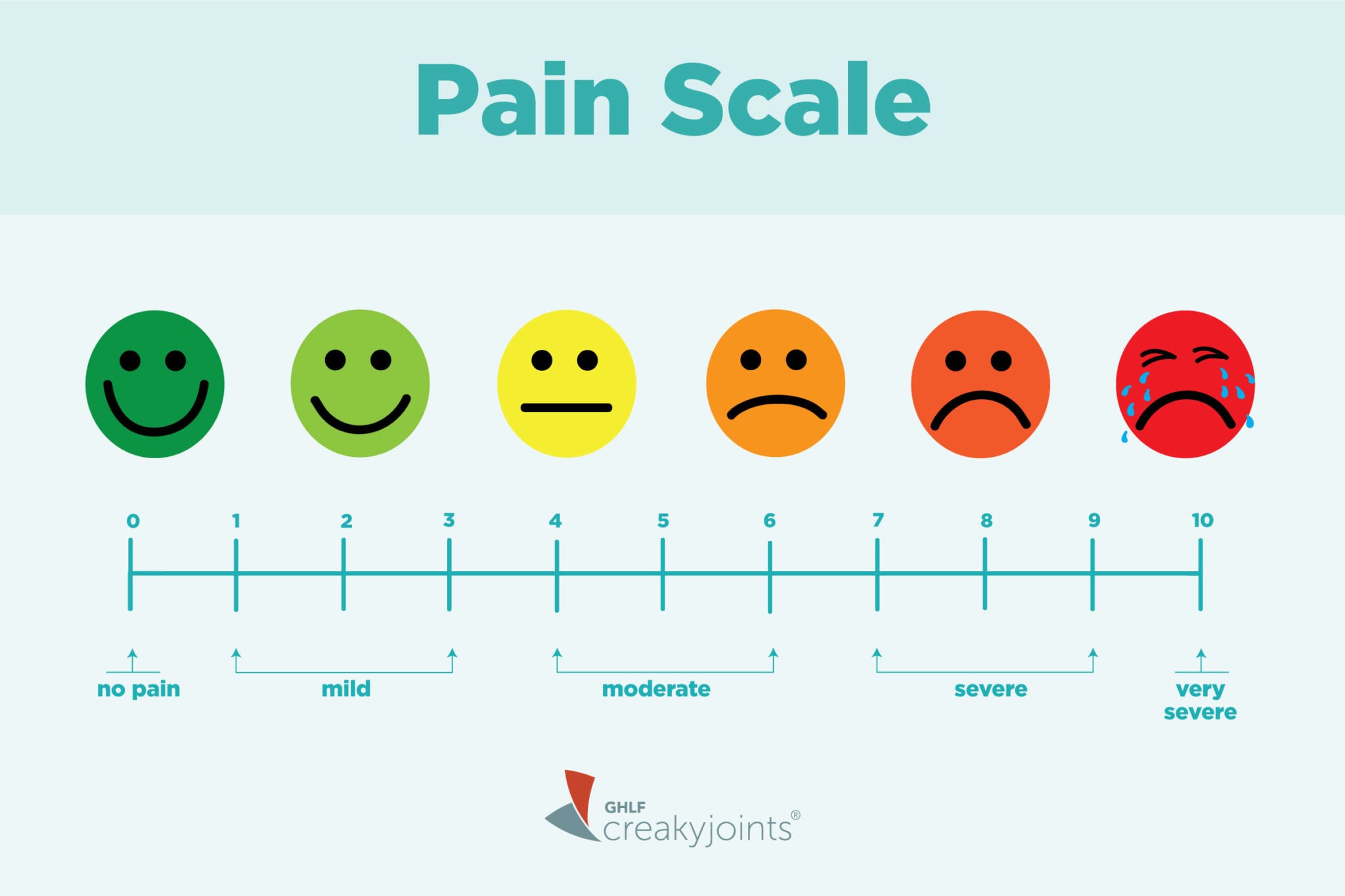
What Is a Pain Scale?
A pain scale is simply a way of rating or quantifying your pain so you can talk about it with your doctor, other health care professionals, or even your friends and family. There are many different kinds of pain scales, but a common one is a numerical scale from 0 to 10. Here, 0 means you have no pain; one to three means mild pain; four to seven is considered moderate pain; eight and above is severe pain.
Pain scales are based on self-reported data — that means from you, the patient — so they are admittedly subjective. Your version of a seven could be someone else’s idea of a three. But the idea is that they can help compare your own ratings over time. Is your pain improving or getting worse? Using a pain scale can also help you and your doctor analyze which factors — a change in physical activity, say, or a new medication regimen — could be responsible for those changes.
The Limitations of Pain Scales
This article from Whyy explains how pain scales came to be such a ubiquitous part of the everyday clinical experience at the doctor’s office or hospital. Perhaps tellingly, the 0-10 scale wasn’t originally intended to help *treat* a patient’s pain; rather, it was created to help researchers study it.
“The primary impetus for the development of the scales we use today was to standardize it, not so much for patients to tell us how much pain they have in the clinical setting, but to standardize it from the perspective of being able to study it for research purposes,” John Farrar, MD, PhD, a pain specialist and director of the Biostatistcs Analysis Center at the University of Pennsylvania, said in the Whyy article.
Numerical pain scales focus on pain severity, but they don’t address other aspects of pain, notes Verywell, “such as qualities of pain (sharp, dull, throbbing) or other characteristics of pain (annoying or unbearable).” There are other questionnaires designed for that purpose.
The New Thinking on Pain Scales
In a recent study, John Markman, MD, director of the Translational Pain Research Program at the University of Rochester School of Medicine and Dentistry, and colleagues studied data from other studies that asked chronic pain patients to rate their pain using both numbers and words, NPR recently reported.
Patients were asked to rate their pain on a scale of 0 to 10 and were also asked the question, “Is your pain tolerable?”
The researchers found that about 75 percent of patients who rated their pain between four and seven on the numerical scale, which is a range that usually demands higher medication doses, also said their pain was “tolerable,” which is a word that typically indicates no need for more pain treatment, according to NPR.
The discrepancy shows the problem with doctors relying only on numbers without additional data. When patients also use words to talk about their pain and how it affects their daily lives, they can paint a more complete and precise picture for their doctors.
More Ways of Assessing Pain
Another way to communicate your pain and the ways it affects your daily life with your doctor is through something called patient-reported outcomes, or PROs. Rather than filling out, say, a 0-10 pain scale at a single point in time (such as during a doctor visit), tracking PROs regularly — such as in a smartphone app — can let patients record key symptoms, analyze how their symptoms are interfering with specific aspects of their daily life, and attempt to marry that data with other variables, such as medication changes, sleep, physical activity, and more.
ArthritisPower® is one example of a PRO app that lets people living with arthritis and related conditions track their symptoms, treatments, medications, and health data with their iPhone or Android (via app) and their computer.
Doctors are increasingly using PRO tools to help get a bigger picture of their patients’ health.
At the same time, new medical technology may help doctors quantify pain without relying only on patients’ self-reported data, according to this American Psychological Association article. Various researchers are studying how functional magnetic resonance imaging (fMRI) can show patterns of brain activity associated with pain, as well as how certain immune system biomarkers (via blood tests) could indicate the presence of pain. Tools that measure pupil response and facial movements (such as looking at people’s grimaces and winces) are also currently being studied.
How to Talk About Your Pain
Even if your doctor uses a 0-10 pain scale, consider these additional ways to discuss your pain to be more precise.
- Compare your pain with the worst pain you’ve ever experienced. Ever given birth, experienced kidney stones, or endured a significant trauma, like a bad fracture? Comparing your chronic pain with the worst pain you’ve ever had can help add perspective, according to Chrystina Jeter, MD, an anesthesiologist and pain management specialist with UCLA Health, in the NPR article.
- Put your pain in the context of your daily activities. Does it get better or worse when you do physical activity or exercise? How is your pain in the morning or at night?
- Talk about how your pain affects your function. Does your pain prevent you from doing specific activities that you used to be able to?
Sharing these qualitative details with your doctor can help paint a more accurate picture of your pain beyond the 0-10 scale. This can help ensure you get the best treatment possible.
Related Resources
Check out our recent webinar with Yale researcher William C. Becker, MD, about the opportunities and challenges when it comes to pain management.
Learn More About ArthritisPower
This question was one of our bi-monthly ArthritisPower Community Questions, offering ArthritisPower participants an opportunity to learn from each other and provide our research team insights.
If you’re diagnosed with RA or a musculoskeletal condition, participate in future polls like this, as well as research studies, by joining CreakyJoints’ patient research registry, ArthritisPower. As a patient-led, patient-centered initiative, our research team is committed to investigating research topics that matter most to you.
If you enjoyed reading this article, you’ll love what our video has to offer.