

If you’re reading this, chances are you have a strong suspicion that you have ankylosing spondylitis (AS), a type of inflammatory autoimmune arthritis that predominantly affects the spine and sacroiliac (SI) joints. Maybe it’s because you’ve checked out PainSpot, you’ve been Googling your symptoms, or you’ve already visited your primary care doctor and got a referral to see a rheumatologist. Perhaps you have family members with AS who’ve encouraged you to see a doctor because your symptoms are similar.
Whatever the reasons for your rheumatologist visit, it’s great that you’re taking this step to get examined. Ankylosing spondylitis is a serious chronic disease that can cause a wide range of complications if left untreated, but it can be treated. There are many different kinds of medications available that can ease your pain and other symptoms and may help stop the progression of the disease.
Seeing a rheumatologist is key. However, keep in mind that not everyone with AS who sees a rheumatologist necessarily has a good experience. Not all rheumatologists have the same level of experience diagnosing and treating people with AS or other kinds of spinal arthritis. Some rheumatologists may be hesitant to even see patients with back pain because they don’t want to treat mechanical back pain, which is far more prevalent than the inflammatory kind that occurs in AS.
“Rheumatologists treat over 100 different rheumatic diseases, so very few are going to be experts in AS,” say Charis Hill, 31, who was diagnosed with AS in 2013. “If you want the best treatment for your body you have to become an expert both in your own body and your own disease, and help rheumatologists learn about your specialty.”
A smart first step when you’re even considering which doctor to see is to ask about their experience treating people with AS. You want to see a doctor who is passionate about treating people with AS or axial spondyloarthritis (a type of inflammatory spinal arthritis that doesn’t present with damage on imaging tests), is up to date on the latest guidelines for testing and treatment, and understands how to manage co-occurring diseases and complications.
Once you have an appointment with a promising rheumatologist in the books, the following tips can help you prepare as best as possible.
1. Start tracking your symptoms closely, if you haven’t already.
“Write down every single thing you’re going through,” says Regan Reynolds, who was diagnosed with ankylosing spondylitis in 2002 at age 22, though she started having symptoms about a decade earlier. “Every little symptom could be related, even if you think it’s not.” When Reynolds first started experiencing pain symptoms (the main one was sharp foot pain that felt like “someone was shoving a pencil in my heel”), she also had gastrointestinal symptoms. At the time, no one connected the dots, but now doctors know that AS and GI complaints are closely related.
“Make symptom notes or use an app like ArthritisPower to track your own health, then give a printed-out version to your nurse or doctor for each visit,” Hill recommends. “These will become part of your patient record and your doctor can’t deny the symptoms you track over time that become part of your chart.”
2. Be able to describe your back pain, hip pain, or other symptoms in as much detail as possible.
One thing your doctor will want to gauge is whether your back pain is inflammatory or mechanical. They’ll do this by asking you questions about what times of day your pain is worse (inflammatory back pain is often worse first thing in the morning); whether your pain feels better or worse when you move around (inflammatory back pain tends to get better with movement and exercise); whether your back pain ever wakes you up at night (mechanical back pain tends not to); and how long your pain lasts (inflammatory back pain tends to last longer than three months but can ebb and flow; mechanical back pain tends to be more acute and hurt consistently for a shorter period of time).
Make sure you point out everywhere on your body you’re experiencing pain. AS doesn’t just strike the back and hips. People with AS often describe something called “alternating buttock pain,” pain in their heels, and pain in their rib cage, for example. It can also affect your knees, neck, and other joints.
“Be honest and forthcoming about your daily life and symptoms,” says Hill. “Don’t show up to appointments looking better than you feel; the last person you want to hide your symptoms from is the very person who is supposed to help treat you.”
3. Bring a list of any medications or supplements you take, or the actual bottles.
It’s a good idea to do this for any type of doctor’s visit you have, so your physician can see what you take regularly and make sure you’re not at risk of any potentially dangerous interactions or dosages. But the drugs you use to treat yourself can also provide a clue about your pain. Ankylosing spondylitis and other types of inflammatory spinal arthritis tend to respond to nonsteroidal anti-inflammatory medication (NSAIDs) such as ibuprofen or naproxen. If your doctor sees that taking these drugs helps you feel better, it could help them get to the bottom of your diagnosis.
4. Ask about any tests you may be likely to get and how may you need to prepare for them.
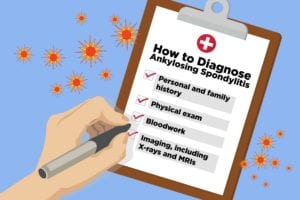
It’s important to know there isn’t a single test (blood test or imaging test) that can clinch an AS diagnosis; as with most rheumatological diseases, your doctor will use a combination of test results, physical exam, and clinical judgment to conclude what you may or may not have. Read more about how doctors diagnose AS here.
That said, if you have multiple signs and symptoms of AS, your evaluation should include a blood test for the HLA-B27 genetic marker, says rheumatologist Doug Roberts, MD, founder of PainSpot. Not everyone with AS tests positive for HLA-B27, and not everyone who tests positive has AS. But if your doctor doesn’t bring it up, you should ask about whether you can get this blood test. “If it is positive, and your symptoms are concerning for AS, your risk of AS goes way up,” he says.
Imaging tests (both X-rays and MRIs) also factor in to getting diagnosed with AS. You can ask before your appointment if you think your doctor will want you to get these tests and if there’s anything you should do to prepare in advance; for example, not eating or drinking for several hours beforehand.
5. Bring a family member or friend to take notes.
Getting to the bottom of a complicated list of symptoms is stressful and confusing. It’s hard to listen to the doctor, write things down, and keep track of all your questions at the same time. Bringing a family member or friend to take notes can relieve some of that burden. It will also help provide an objective perspective on what happened in the appointment.
“A calm, present friend or loved one can help document appointments and be an advocate in the moment to make sure questions are answered and you are treated humanely,” says Hill. She advises bringing checking off questions on your list as your doctor answers them to make sure everything is addressed.
6. Do advance research on treatment options so you can ask questions.
The good news is that ankylosing spondylitis and other types of inflammatory arthritis are treatable and many good treatment options exist. This wasn’t always this case; when Reynolds was diagnosed, her doctor could offer her only NSAIDs, which she wasn’t able to take.
“By the time people get to my office, they’ve usually failed on NSAIDs and I want to put them on a biologic right away,” says Santa Fe-based rheumatologist Hillary Norton, MD, who was diagnosed with AS herself during her medical residency. “It’s a hurdle to encourage people to switch from a drug that’s over the counter to one that’s injectable or infusible, but it’s important for people to know that these medications will allow them to stay active and do what they want to do.”
You can prepare by learning about possible treatments in our ankylosing spondylitis patient guidelines, so you’ll be familiar with your options when your doctor brings them up. Download the free AS patient guidelines here.
Ask your doctor if they have resources they recommend, “so you can do your own research in an environment recommended by a physician,” says Hill.
7. Ask about other types of health care providers you might need to see.
If your doctor suspects you have AS, you may need to start seeing other kinds of care providers in addition to your primary care doctor and rheumatologist. AS tends to co-occur with psoriasis and inflammatory bowel diseases, so your doctor may want you to also see a dermatologist or gastroenterologist. Uveitis, a type of eye inflammation, is also very common, so you will need to start seeing an eye doctor regularly if you’re not already. You may want to see a physical therapist to help you adjust your exercise and physical activity regimen, or a nutritionist to help you make healthy eating lifestyle changes.
On the other hand, if your doctor isn’t sure if you have AS or suspects you have a different health issue, make sure you get clarification on which specialists or care providers to see next.
8. Make sure you know how often you will need follow-up visits and tests.
This will depend on your diagnosis and treatment plan, of course. As a general rule, rheumatologists tend to see patients with AS every three months or so to monitor your progress and make sure your treatment plan is helping to relieve symptoms.
Diagnosing AS can be especially challenging if you don’t test positive for the HLA-B27 genetic marker (and this marker is less common in African Americans and people who are not of European descent) and you don’t have radiographic changes (meaning your X-rays and MRIs don’t show bone or joint damage).
If your doctor isn’t sure whether or not you have AS or another kind of inflammatory arthritis, ask what steps to take and when it may make sense to come back for another evaluation. When Reynolds first saw a rheumatologist in 1998, she was diagnosed with undifferentiated spondyloarthropathy because her doctor couldn’t see any evidence of damage on her X-rays. But she kept returning for follow-up visits every year and she was finally able to be diagnosed with ankylosing spondylitis a few years later.
Of course, with the availability of biologic drugs that can better manage disease progression, people with early-stage spondyloarthritis may never have to progress to ankylosing spondylitis, where damage to the joints has already occurred. This is an ongoing and exciting area of research in rheumatology.
9. Be prepared to accept that you might NOT have AS.
It’s never a good idea to march into your doctor’s office with 50 pages of internet printouts demanding to be diagnosed with what you think you have. Your best bet is to do your research, be able to clearly list out all your symptoms and your medical history, and ask discerning questions of your doctor as they do your physical exam and tests. Pain and systemic symptoms are frustrating and mysterious and getting the right diagnosis boils down to you and a doctor you trust working together as a team to get to the bottom of it.
If your doctor strongly thinks your symptoms are not indicative of AS, then make sure you understand why they’ve come to that conclusion, and so…
10. Don’t leave until your doctor shares what he or she thinks is going on.
“Everyone hurts.” “Just try some ibuprofen.” “You can’t have AS, you’re too young.” “Well, that’s just getting older.” “When was your last period? Your back hurts because of that.” “Exercise more.” “Change your diet and you’ll feel better.” If your provider is saying things like this, it could be a sign they’re dismissing your symptoms without a thorough-enough examination, say Hill and AS patient Jed Finley. This is something many patients in our CreakyJoints community report during their journey to diagnosis.
“Don’t let your doctor get away with these lines,” says Finley, 37, who notes another big red flag is if your doctor attempts to diagnose you from across the room without really touching you or examining your joints. “Don’t let anyone invalidate your pain. Even if you’re not feeling a ‘9’ on a ‘0-10 scale’ you are still in pain. Nobody should have to live in pain like this.”
A good question to ask, especially if your pain is dismissed as simple chronic back pain, advises Dr. Roberts: Can you be 100 percent sure I don’t have early-stage ankylosing spondylitis without additional testing or consultations? Be open to hearing what they have to say, but make sure you received a thorough physical exam, bloodwork, and imaging tests before moving on.
Keep Reading
- How Doctors Diagnose Ankylosing Spondylitis: What to Expect at the Rheumatologist
- 12 Ankylosing Spondylitis Symptoms You Can’t Afford to Ignore
- 7 Tips You Need to Beat Arthritis Fatigue





