A textbook definition of rheumatoid arthritis (RA) involves its effects on the joints: Rheumatoid arthritis is an autoimmune disease where your immune system mistakenly attacks the joints. That leads to inflammation that causes the tissue lining the inside of the joints to thicken, leading to swelling and pain in and around the joints.
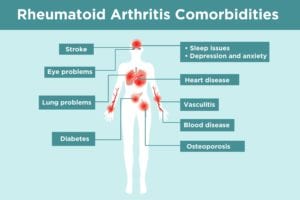
But rheumatoid arthritis is not *just* a disease of the joints. The inflammation in RA is what’s known as “systemic,” which means that rheumatoid arthritis can affect many different parts of the body and cause additional health problems. A mainstay of RA treatment is trying to prevent such complications, also known as comorbidities.
“The primary goal of RA therapy is to reduce pain, swelling, and stiffness, which improves function,” says Brett Smith, DO, a rheumatologist with Blount Memorial Physicians Group in Alcoa, Tennessee. “But if we don’t treat the disease aggressively, it can also increase the risk of heart disease, bone fracture, and other problems. It’s not all about pain.”
As a patient, it’s important to understand all the possible rheumatoid arthritis comorbidities and complications so you can try to prevent them and watch for early signs and symptoms. “I always discuss potential scenarios with my patients,” says Anand A. Kumthekar, MD, a rheumatologist who practices at the Montefiore Medical Center in Bronx, New York. “Then they can be on the lookout for symptoms and get the appropriate testing and referral to the right specialist if need be.”
Even though the list of RA complications can be long and alarming, this is important to know: “Treating the rheumatoid arthritis effectively helps minimize long-term complications,” says Dee Dee Wu, MD, an assistant attending physician at Hospital for Special Surgery in Paramus, New Jersey.
Once you read through this list of rheumatoid arthritis complications, bring up any questions or concerns you have with your doctor. You may need to create a health care team of different specialists, such as seeing a rheumatologist and a cardiologist — or facilitate better communication between them to ensure you’re getting optimal care for your rheumatoid arthritis and its comorbidities.
Common Rheumatoid Arthritis Comorbidities

1. Rheumatoid Arthritis and Heart Disease
Heart disease is a catch-all term that includes atherosclerosis (the build-up of plaque in the arteries), heart attack, and irregular heartbeat. Heart disease is the leading cause of death in rheumatoid arthritis (RA) patients. If you have RA, you have a twofold increased risk for heart attack and stroke. For people who’ve had RA for 10 years or more, the risk rises to nearly threefold. Rheumatoid arthritis patients may also develop congestive heart failure, where the heart can’t pump enough blood to the rest of the body and fluid collects in the lungs.
“Several mechanisms are responsible for the increased risk of cardiovascular disease in rheumatoid arthritis,” says Bryant England, MD, a rheumatologist who practices at the University of Nebraska Medical Center and Veterans Affairs Nebraska-Western Iowa Health Care System in Omaha, Nebraska. “These include inflammation, changes in cholesterol levels and function, and a high potential for co-occurring risk factors, such as diabetes and high blood pressure.”
RA-related inflammation narrows blood vessels and leads to plaque formation inside of the arteries. If this plaque clogs blood vessels, heart attack or stroke may result. Inflammation can also reshape the blood vessel walls, making the plaque inside the vessels more prone to rupture, which can also trigger a heart attack. Cholesterol levels are more likely to be unstable in people with higher levels of inflammation and RA disease activity. This can lead to an even higher risk of heart attack for people with RA.
In addition, some medications used for arthritis, such as prednisone and NSAIDs, can increase heart disease risk, while other arthritis drugs offer heart protective benefits (including TNF inhibitors, methotrexate, and hydroxychloroquine).
It’s crucial to get control of RA as early as possible after diagnosis, and to assess risk factors for heart disease when the patient is diagnosed with RA to prevent further cardiovascular damage.
To help reduce the risk of heart disease and stroke, doctors will suggest that you stop smoking, lose weight, maintain normal cholesterol levels, exercise, and eat healthy foods. “It’s important to treat rheumatoid arthritis aggressively with medications to reduce the risk of developing cardiovascular disease,” says Dr. England.
Read more about managing heart disease risk in rheumatoid arthritis.
2. Rheumatoid Arthritis and Stroke
Contrary to popular belief, stroke does not just happen to the elderly. Anyone can have a stroke, which happens when blood flow to an area of the brain is reduced or cut off, causing brain cells to die. This occurs either because a blood clot blocks the blood flow or a blood vessel leaks or bursts. Symptoms of stroke can include slurring speech, confusion, paralysis or numbness of the face, arm or leg, a sudden severe headache, trouble seeing in one or both eyes, and difficulty walking.
Along with heart attack, stroke is the cause of many premature deaths in people with rheumatoid arthritis (RA). One study found that people with RA had a 67 percent higher risk of stroke than those without, though it remains unclear to what extent arthritis is an independent risk factor for stroke. The connection appears to be inflammation. Similar to heart disease, some studies show that inflammation increases a person’s risk for stroke.
Additional risk factors for stroke include high cholesterol, diabetes, obesity, smoking, high blood pressure, and carotid artery disease (in which the carotid arteries in your neck, which supply the brain with blood, become narrowed due to the build-up of plaque). If someone with RA has any of these other conditions, the risk of stroke becomes even higher.
People with RA should take care to reduce their risk of stroke, along with all forms of heart disease, by addressing risk factors they can control: not smoking, losing weight, having healthy cholesterol levels, eating a balanced diet, and exercising.
3. Rheumatoid Arthritis and Lung Problems
People with rheumatoid arthritis are at risk for inflammation and scarring of the lung tissues. “It’s not fully understood why it happens, but it’s believed to be a combination of environmental exposure, like tobacco smoke, active rheumatoid arthritis, and accelerated aging process,” says Dr. England. Lung problems that occur in people with rheumatoid arthritis include:
Rheumatoid arthritis-associated interstitial lung disease (RA-ILD) is a group of lung disorders marked by inflammation and scarring of the lung tissue, which is caused by the immune system attacking the lungs. As scarring becomes more severe it can affect breathing and lead to breathlessness and dry cough.
Rheumatoid nodules can occur in the lungs of patients with RA. Read more about rheumatoid nodules and how to manage them.
Pulmonary fibrosis is permanent scarring of the lungs, often linked with RA-ILD. As healthy air sacs are replaced by scar tissue, breathing becomes difficult. Oxygen therapy may make breathing easier, but it cannot undo the damage caused by the scarring.
Pleurisy is inflammation of the lining of the lungs, called the pleura. It occurs in more than half of all people with RA and can make breathing painful.
Some drugs used to treat rheumatoid arthritis, such as methotrexate, may cause inflammation in the lining of the lungs. “Fortunately, these medication complications are quite rare,” says Dr. England. For most rheumatoid arthritis patients, the benefits of methotrexate far outweigh the risk of its role in lung problems, says Arthur Mandelin, MD, PhD, associate professor of medicine at Northwestern University in the Feinberg School of Medicine.
Signs of lung problems in rheumatoid arthritis include persistent cough, shortness of breath that worsens, and chest pain. “If there are any red flags, I would do a screening chest X-ray and possible CAT scan of the chest,” says Dr. Wu. “If either tests are abnormal, I’d refer you to a pulmonologist for further evaluation. Treatment depends on the severity of the complication.”
Smoking increases the risk of lung problems, so work with your doctor to devise a smoking cessation plan, says Dr. England. “Rheumatoid arthritis in a smoker is harder to control than rheumatoid arthritis in a nonsmoker,” says Dr. Mandelin.
Read more about how arthritis affects the lungs and how to protect your lung health.
4. Rheumatoid Arthritis and Eye Problems
Rheumatoid arthritis raises the risk for different kinds of eye issues, including dry eye and inflammation-related eye problems.
Dry eye
“Dry eye is one of the most common complications of rheumatoid arthritis,” says Dr. Kumthekar. Many people with rheumatoid arthritis also have another autoimmune disease called Sjögren’s syndrome, in which your immune system attacks moisture-producing cells like the salivary and tear glands, causing dry eye.
Long-term eye dryness can lead to scarring, ulceration, infection, and perforation of the cornea. “Aggressive treatment of rheumatoid arthritis, topical eye drops, and consulting with an ophthalmologist is essential to preserve vision and prevent eye problems,” says Dr. England.
Medications that can treat this condition include pilocarpine (Salagen) and cevimeline (Evoxac), which are taken in pill form, says Dr. Mandelin. Cyclosporine (Restasis) or lifitegrast (Xiidra) eye drops are often used.
“However, the most important treatment for Sjögren’s syndrome isn’t prescription medication,” says Dr. Mandelin. “The affected area needs its moisture replaced. Over-the-counter wetting eye drops, as well as hydrating mouthwashes, vaginal lubricants, or skin moisturizers, depending on where the dryness is, are the cornerstones of therapy.”
Eye inflammation
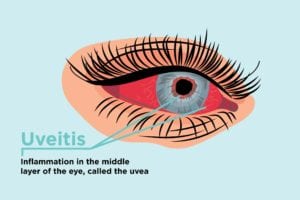
Rheumatoid arthritis may also cause inflammation of the eyeball itself, called iritis, uveitis, or scleritis, depending on which part of the eyeball is affected, says Dr. Mandelin. Symptoms include pain, redness, and blurry vision.
“Where dry eye from Sjogren’s syndrome tends to be mild in the short term and its major effects on health usually happen later due to the chronic nature of the irritating dryness, uveitis and related conditions can lead to trouble quickly because the eye itself is inflamed,” says Dr. Mandelin. “These symptoms shouldn’t be ignored. If you think you have uveitis, get medical attention right away.”
Read more about uveitis and arthritis.
5. Rheumatoid Arthritis and Vasculitis
Some people with RA get rheumatoid vasculitis, where blood vessels become inflamed. This complication weakens and narrows blood vessels. It’s rare; only about 5 percent of people with rheumatoid arthritis develop rheumatoid vasculitis, thanks to improved therapy and disease management. The most common signs of vasculitis are leg ulcers and sores around or under your fingernails. Since rheumatoid vasculitis can affect the hand and feet nerves, you may get a burning, tingling, or numb sensation. “Aggressive treatment of the joint pain and swelling reduces the risk of developing rheumatoid vasculitis,” says Dr. Smith.
Read more about diagnosing and treating rheumatoid vasculitis.

6. Rheumatoid Arthritis and Sleep Issues
Difficulty getting a restful night’s sleep is common in rheumatoid arthritis. Pain from rheumatoid arthritis can wake people during the night, preventing a good sleep. And in a vicious cycle, getting too little sleep can also exacerbate RA symptoms like pain and fatigue.
You and your doctor should discuss why you’re waking up at night and figure out strategies to help you sleep better. It may be the case that rheumatoid arthritis medication is contributing to your difficulty sleeping and you may need to change which drugs you take or when you take them. Corticosteroids such as prednisone may affect your sleep, for example. “You could take prednisone only in the morning, rather than twice a day,” says Dr. Wu.
“Sleep is crucial in reducing pain levels,” says Dr. Smith. He says that moderate intensity exercise helps promote sleep and improve sleep quality while also helping joint function. If you have difficulty falling asleep, he recommends keeping your bedroom cool and avoiding caffeine in the evening. Here are other solutions to help achieve a better night’s sleep with arthritis.

7. Rheumatoid Arthritis and Mental Health
Rheumatoid arthritis is a lifechanging, lifelong disease with a significant impact on mental health. Depression, anxiety, and stress are very common along people managing chronic illness and rheumatoid arthritis is no exception. Research shows that people with rheumatoid arthritis (RA) are twice as likely to have depression as those without RA. Anxiety can be just as big of an issue in arthritis as depression. In fact, a CDC study found that anxiety was even more common in RA patients than depression.
Depression and anxiety in rheumatoid arthritis can be due to a number of factors, including being in chronic pain, experiencing inflammation that can affect your mood, and having your lifestyle impacted by your disease (for example, how RA can affect your ability to work, maintain relationships, and do your normal activities and hobbies).
Depression and anxiety are not just “feeling sad” or “feeling worried” — these are diseases that affect your brain chemistry and behavior. It is critical to recognize signs that you might have depression, anxiety, or excessive stress, such as:
- Sleep problems (sleeping more or less than usual)
- Appetite changes (eating more or less than usual)
- Fatigue
- Irritability
- Anger
- Feeling hopeless
- Feeling helpless, worthless, or guilty
- Difficulty concentrating or focusing
- Physical symptoms, such as headaches or digestive distress (cramps or upset stomach)
Let your doctor know how you’re feeling. You may need medication or therapy to help manage your mental health.
Read more about coping with depression and arthritis.
8. Rheumatoid Arthritis and Blood Disease
Rheumatoid arthritis can cause anemia, a reduction in red blood cells. Anemia can cause rapid heartbeat, fatigue, shortness of breath, dizziness, leg cramps, and insomnia. Another complication from rheumatoid arthritis is thrombocytosis, in which inflammation leads to high levels of platelets in your blood. Platelets help your blood clot. Too many platelets, though, can lead to stroke, heart attack, or blood vessel clots. Speak with your health care provider if you have any of these symptoms. They may need to adjust your medications to control these conditions.
Read more about rheumatoid arthritis and anemia.
9. Rheumatoid Arthritis and Osteoporosis
Rheumatoid arthritis increases the risk for osteoporosis, a condition that weakens your bones and makes them more susceptible to fractures. One reason is because rheumatoid arthritis patients often use corticosteroid medication, which weakens bones as a side effect. Symptoms of an osteoporotic fracture include back pain, change in posture or curvature of the spine, or broken bones from a fall, especially in the wrist or hip.
“Bone loss can be prevented by doing weight-bearing exercise as well as taking calcium, vitamin D, or osteoporosis medications to prevent bone loss or rebuild bone,” says Dr. England. “Because osteoporosis is often asymptomatic, talk to your health care provider about how often to get bone density scans, which can help determine if you have osteoporosis before you experience a fracture.”
Read more about rheumatoid arthritis and osteoporosis.
10. Rheumatoid Arthritis and Diabetes
Diabetes occurs when the body is unable to produce hormone insulin (type 1 diabetes) or use it sufficiently (type 2 diabetes). Insulin converts the sugars we get from food into energy. Type 1 diabetes is an autoimmune disease in which the body’s immune system attacks the cells of the pancreas that make insulin. Type 2 diabetes is a metabolic disorder that affects the way the body utilizes insulin.
Having rheumatoid arthritis raises your risk for diabetes and having diabetes increases your risk of developing arthritis, but there’s a lot we still don’t know about the connection between diabetes and rheumatoid arthritis.
One theory suggests that RA inflammation may play a role in the development of diabetes. Insulin resistance tends to be elevated in RA, and levels of inflammatory markers tend to be high both in people with RA and people with diabetes. Another theory is that people with RA and other forms of arthritis tend to be more sedentary, and a sedentary lifestyle leads to obesity, a known risk factor for type 2 diabetes.
Medications used for arthritis could also play a role, as it is well known that steroids can raise blood sugar levels. However, other RA drugs may lower diabetes risk: the drug hydroxychloroquine is associated with a lower risk of diabetes among people with RA, though it’s unclear why this is so. Other RA drugs known as TNF blockers and methotrexate have been shown to improve insulin resistance and lower diabetes risk, but more research is needed.
For people with RA who are concerned about diabetes, it is important to maintain a healthy lifestyle. This includes exercise, eating a healthy diet that contains a balance of protein, healthy fats, whole grains, and non-starchy vegetables, maintaining a healthy weight, and not smoking. These choices not only help manage RA; they also are important to reduce your risk of diabetes.
Keep Reading
Subscribe to CreakyJoints
Get the latest arthritis news in your inbox. Sign up for CreakyJoints and hear about the latest research updates and medical news that could affect you.