Tracking your RA pain can help you better understand your condition and talk about it with your doctor. Join ArthritisPower, a patient-centered research registry, to learn more about your RA. Sign up here.
Inflammation is the root cause of rheumatoid arthritis (RA) pain — but it’s certainly not the only cause. In fact, many people with RA experience joint pain without swelling and other types of pain, in spite of having low levels of inflammation, few affected joints, and low disease activity.
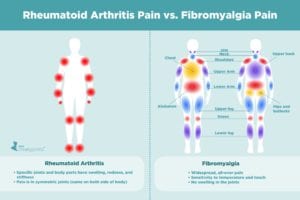
Rheumatoid arthritis is a chronic, inflammatory autoimmune disorder in which the body’s own immune system attacks the lining of the membranes that surround the joints (the synovium). It often causes pain, stiffness, and swelling of multiple joints on both sides of the body.
However, it is possible to have RA and experience pain for other reasons at the same time.
“If a rheumatologist and RA patient have a mutual understanding that the rheumatoid arthritis is in remission, then we need to explore why the patient is still having pain,” says Elizabeth Schulman, MD, a rheumatologist at Hospital for Special Surgery in New York City.
Although figuring out the root cause of pain can feel like a guessing game — if it’s not RA, what else could it be? — there are several other common conditions that should be considered.
“Other issues can cause pain in people with RA beside rheumatoid arthritis, which is important to remember,” says rheumatologist Angus Worthing, MD, a clinical assistant professor of medicine at Georgetown University Medical Center in Washington, D.C. “Broken bones, torn or sprained muscles or tendons, carpal tunnel syndrome, sudden muscle strain in the low back or neck, tendinitis, and bursitis — they all happen to people with RA, but might not be caused by RA.”
Lack of sleep (sometimes referred to as painsomnia) and depression can also certainly be part of the pain equation. It’s a vicious cycle, says Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida. “Pain creates insomnia, which leads to more pain, which contributes to depression, which then affects pain,” he says.
Here is a look at some common co-occurring conditions that you may mistake for RA pain, along with what you can expect if RA isn’t the only medical issue you’re trying to treat.
Osteoarthritis (OA)

Osteoarthritis is a condition in which the cartilage that cushions a joint wears away, causing pain and stiffness. It typically occurs later in life (usually after age 50) though it may start earlier, especially if your joints have become damaged by rheumatoid arthritis or injury. This is called secondary OA, notes Leah Alon (Nichols), MD, a rheumatologist in New York City. Secondary osteoarthritis can also occur after a joint injury.
The risk of someone with RA developing primary OA, which occurs with age and joint use but has no underlying causes, is the same as the general population. Primary OA occurs in joints unaffected by inflammatory arthritis.
OA is characterized by abnormalities in all of the tissues in the joint, leading to symptoms and loss of normal joint function. “OA sometimes affects different joints than RA, including the base of thumb, one or the other knee or hip, the big toe, and DIPs of hands,” says Dr. Worthing.
The distal interphalangeal joint (DIP) joint is located at the tip of the finger, just before the nail starts.
“OA is generally stiff for less than 30 minutes in the morning, and may lead to only bony but not soft swelling,” Dr. Worthing continues. “OA classically causes ‘gel’ phenomenon in which a joint may feel stiff, sore, or aching for a short time after rest, like when you have to ‘walk off’ knee pain after prolonged sitting or standing.”
By contrast, RA usually affects the metacarpophalangeal (MCP) and proximal interphalangeal (PIP) joints, is symmetric, and causes more prominent morning stiffness and pain, he adds. The MCP joint is where the hand bone (the metacarpal) meets the finger bones (the phalanges). The PIP joint (PIP joint) is located between the first two bones of the finger (near where your knuckles are).
If your rheumatologist suspects you could have OA, a physical exam and X-ray can be used to diagnose OA. “It’s important to diagnose OA because it helps distinguish when OA is causing joint pain instead of RA,” says Dr. Worthing.
How This Affects Treatment
In this case, RA medication won’t need to be escalated, and OA pain can be treated with pain relief measures, Dr. Worthing says.
Treatment for OA includes non-steroidal anti-inflammatory drugs (NSAIDs) and acetaminophen (Tylenol) to control pain and inflammation, as well as steroid injections in an affected joint.
Fibromyalgia
Fibromyalgia, a chronic pain condition characterized by fatigue and pain all over the body, is common in people with rheumatoid arthritis, says Dr. Schulman. In fact, a 2019 study published in the journal Best Practice & Research Clinical Rheumatology cites that between 18 percent and 24 percent of people with RA also have fibromyalgia.
This might be due to changes in the way the nervous system perceives and processes pain in people with RA, which can trigger fibromyalgia.
While someone with RA can often point to a specific body part (like the hand) that has swelling, redness, and stiffness in addition to pain, someone with fibromyalgia tends to experience widespread pain and tenderness at soft tissues, and pain in multiple organ systems (headaches, abdominal pain, sinus, or urinary tract pain), explains Dr. Worthing. Unlike RA, there is no swelling in the joints with fibromyalgia.
Many patients describe fibromyalgia pain as “catastrophic,” he adds, and some may experience tingling or burning sensations in areas of the body as well as significant fatigue, disturbed sleep, difficulty concentrating or remembering things (fibro fog), and depression. Fibromyalgia could make you overly sensitive to temperature and touch.
Fibromyalgia is a challenging disorder to diagnose because there’s no single test (such as a blood test or an imaging test like an X-ray) that can confirm a diagnosis. Rather, fibromyalgia is considered a “diagnosis of exclusion,” which means doctors need to first rule out other health problems.
If your rheumatologist suspects fibromyalgia, they will listen to your history and symptoms, including their severity and duration, and may do a physical exam to check for painful areas and tender points.
How This Affects Treatment
“Fibromyalgia can be treated with graded gentle exercise, adequate sleep, medications that affect pain neurotransmitters, such as muscle relaxants, antidepressants, and drugs that are or are similar to antiseizure drugs, and cognitive behavioral therapy,” says Dr. Worthing.
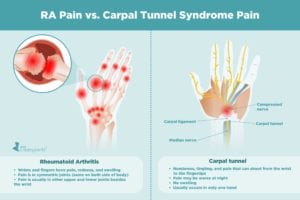
Carpal Tunnel Syndrome
Carpal tunnel syndrome (CTS) occurs when a major nerve in the hand — the median nerve — becomes compressed in the carpal tunnel, a narrow passageway on the palm side of your wrist that also houses the tendons that bend the fingers.
“If your wrist joint swells with RA, it’s a very narrow canal there, and the swelling can press the nerve and you get carpal tunnel syndrome,” says Dr. Alon. “You have to treat the swelling from the RA to make that type of carpal tunnel better.”
In addition to RA, a number of health problems can also cause swelling of this area, including diabetes, thyroid issues, and hormonal changes that occur during pregnancy. Injuries, such as a wrist fracture, can also contribute to the onset of carpal tunnel syndrome.
Both RA and CTS affect the hands and wrists, but RA usually affects other areas of the upper and lower body in addition to the wrist area, says Dr. Worthing. RA is also usually present in both hands, while CTS can occur in only one, typically a person’s dominant hand.
“CTS causes numbness, tingling, and pain that can shoot down to the fingertips,” says Dr. Worthing. “RA causes pain that is aching, stiff, or sore.” Pain from CTS may also be worse at night, and unlike RA, there is no swelling.
To diagnose CTS, your rheumatologist will perform a physical exam of the wrist joint (tapping the inside of your wrist, or asking you to bend your wrist down for minute), and do an ultrasound testing of the nerve, or EMG (electromyography), which measures electrical activity of the nerve.
How This Affects Treatment
“If RA is causing the CTS, RA therapy can be escalated or a cortisone injection can be given,” says Dr. Worthing. If CTS exists unrelated to RA, it is often treated with physical therapy, splinting, pain medication, cortisone injection, or surgery in less common cases.
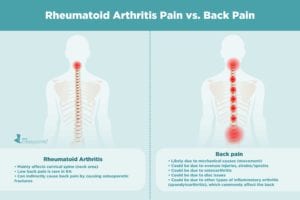
Back Pain
Some people with RA report experiencing back pain, but if lower back pain is your primary pain symptom, it’s likely not due to RA.
“Sometimes patients say that parts of their spine hurt,” says Dr. Alon. “RA can affect the cervical spine [the neck area] but it does not affect the lower spine.”
This is because your lower back does not have synovium, the thin membrane that lines your joints, which gets inflamed with RA.
“Chronic low back pain is virtually impossible from rheumatoid arthritis,” says Dr. Domingues. “The only joint in the back with synovium is the atlanto-occipital joint,” which is located between the base of the skull and the cervical spine.
RA may indirectly affect the back because it increases a person’s risk of developing osteoarthritis and osteoporosis, which can both result in back pain. In most cases, however, low back pain is likely mechanical pain — triggered by the movements of the body, says Dr. Worthing.
If your back has been bothering you, consider your recent activities before chalking up your pain to RA. Did you overdo it at the gym? Did you lift something heavy? Have you been painting your home? Communicating these types of activities known to cause back pain can help your rheumatologist make a diagnosis and recommend treatment.
How It Affects Treatment
The best way to treat mechanical back pain is to allow time to let things heal, try physical therapy, and use pain relief measures like NSAIDs or heat or ice therapy. Lifestyle changes, including losing weight, quitting smoking, improving posture, and exercising more, as well as steroid injections may also be recommended. Surgery is considered a last resort.
Bursitis
Bursitis is a painful condition that occurs when small, fluid-filled sacs — called bursae — that cushion the bones, tendons, and muscles near your joints become inflamed.
“Bursitis is caused by inflammation, but it’s not inflammation in the joints,” says Dr. Domingues. “It’s inflammation in the adjacent tissue called bursa.” Having RA slightly raises your risk of having bursitis, he notes.
Bursitis commonly affects the shoulder, elbow, hip, and knee, and is often caused by repetitive motions or positions that put pressure on the bursae around a joint. “You’ll feel pain when you walk or use your shoulder,” explains Dr. Domingues.
Although RA tends to be a small-joint disease, it can spread to both of your hips as the disease progresses. Inflammatory arthritis in your hip will feel painful and stiff, be worse in the morning, and gradually improve with activity. Hip joint issues may also manifest as groin pain.
“True hip pain from trochanteric bursitis hurts more with movement and when pressure is applied (sleeping on your side) and causes pain in the lateral side of your hip and thighs,” says Dr. Domingues.
If your rheumatologist suspects bursitis, you’ll likely undergo a physical exam to test for tenderness as well as imaging (X-rays or MRI) and lab tests (examining fluid from the bursa) to rule out other problems causing your pain.
How It Affects Treatment
Bursitis treatment can include rest, ice, and anti-inflammatory medications as well as steroid injections if the pain does not subside after a week.
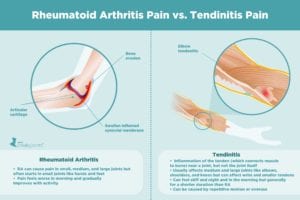
Tendinitis
While RA can cause soreness of tendons and ligaments due to inflammation in the connective tissues in and around the joints, painful tendons are likely a sign of tendinitis (also spelled tendonitis).
“Tendinitis is an overuse syndrome that causes inflammation and stiffness in the tendons,” says Dr. Domingues. The condition is most common in those over age 40 and athletes. In fact, many forms of tendinitis are named after sports — for example, tennis elbow, golfer’s elbow, pitcher’s shoulder, swimmer’s shoulder, and jumper’s knee. People with such conditions as RA, osteoarthritis, gout, and diabetes are also more likely to develop tendinitis.
Unlike RA, which typically causes pain in the hands, wrist, and feet, tendinitis affects the medium and large-size joints, he adds, including the elbow, around the rotator cuff (the shoulder), and thigh.
Another difference between tendinitis and RA is the progression of the pain. “With RA, you feel worse in the morning, but with tendinitis you’ll start the day okay and feel more pain as you move,” says Dr. Domingues.
If your rheumatologist suspects tendinitis, they’ll perform a physical exam and listen for a “creaky sound” that indicates the tendon sheath is inflamed. Imaging tests, including an MRI, will also be done to look for swelling of the tendon sheath.
How It Affects Treatment
Tendinitis is typically treated with rest, physical therapy, splints or braces, over-the-counter NSAIDs, and corticosteroid injections. Surgery may also be an option if the tendon ruptures.
The bottom line: There are multiple conditions that can cause joint paint (or what may be mistaken for joint pain) that can co-occur with rheumatoid arthritis. By verbalizing exactly where on your body you experience pain, and describing how it feels, what brings it on, how long it lasts, and what, if anything, makes it feel better, you can help your rheumatologist take the guesswork out of diagnosing and treating your pain.
Keep Reading
- Rheumatoid Arthritis Pain and Flare-Ups: What to Know and Do
- How to Discuss Your Rheumatoid Arthritis Pain During a Telehealth Visit
- Rheumatoid Arthritis Pain: 7 Things You Should Tell Your Rheumatologist
- Rheumatoid Arthritis Pain: When to Consider a Medication Change
Track Your RA Pain with ArthritisPower
ArthritisPower is a patient-centered research registry for joint, bone, and inflammatory skin conditions like rheumatoid arthritis. You can select different health assessments that matter to you, and choose how often you want to take them. When you have an upcoming doctor appointment, you can discuss your latest assessments and feel more informed. Learn more and sign up here.
This article is part of A Patient’s Guide to Understanding Rheumatoid Arthritis Pain and was made possible by a grant from Sanofi Genzyme.
Feldon P, et al. Carpal Tunnel Syndrome in Rheumatoid Arthritis. Techniques in Orthopaedics. March 2006. https://doi.org/10.1097/01.bto.0000220073.29489.6c.
Interview with Angus Worthing, MD, rheumatologist and clinical assistant professor of medicine at Georgetown University Medical Center in Washington, D.C.
Interview with Elizabeth Schulman, MD, rheumatologist at Hospital for Special Surgery in New York City
Interview with Leah Alon, MD, rheumatologist in New York City
Interview with Vinicius Domingues, MD, a rheumatologist in Daytona Beach, Florida
Kim H, et al. Fibromyalgia Predicts Two-Year Changes in Functional Status in Rheumatoid Arthritis Patients. Arthritis Care & Research. December 2017. doi: https://doi.org/10.1002/acr.23216.
Zhao SS, et al. The prevalence and impact of comorbid fibromyalgia in inflammatory arthritis. Best Practice & Research Clinical Rheumatology. June 2019. doi: https://doi.org/10.1016/j.berh.2019.06.005.