If you have been experiencing warmth, redness, and excruciating and sudden pain in your big toe overnight or first thing in the morning, gout could be to blame. Gout, a form of arthritis that impacts 8.3 million American adults, causes a sudden onset of joint pain and inflammation that can impact your range of motion and ability to perform daily activities.
Some people in the middle of a gout flare report the pain being so severe that they can’t bear to have a bedsheet touch their toes and find it hard to walk around.
What Is Gout, Exactly?
Gout is a condition where excess deposits of a crystalline form of uric acid cause medical problems, says Theodore R. Fields, MD, a rheumatologist at the Hospital for Special Surgery in New York City. Uric acid is a normal byproduct of metabolism; you produce it all the time and excrete it through urine. But when your body produces too much uric acid — medically termed hyperuricemia — it can crystallize and accumulate in your joints, causing gout symptoms including joint pain and kidney stones.
“The most common problem is gouty arthritis, where a person suffers from inflammation in a joint,” Dr. Fields says. “Uric acid crystals can also form in the kidney and cause kidney stones, and can also build up in various locations, such as below the skin.” These large, visible bumps below the skin are known as tophi.
As with most conditions, early diagnosis and prompt treatment are key for feeling your best and preventing any complications, including permanent bone and joint damage as well as an increased risk of many other health problems.
If you put off seeing your doctor, your gout flares can become more frequent and start to affect other joints. You’ll also increase your risk of developing chronic gouty arthritis, which can lead to permanent joint damage, joint deformity, and persistent pain. Read more here about how gout can progress over time.
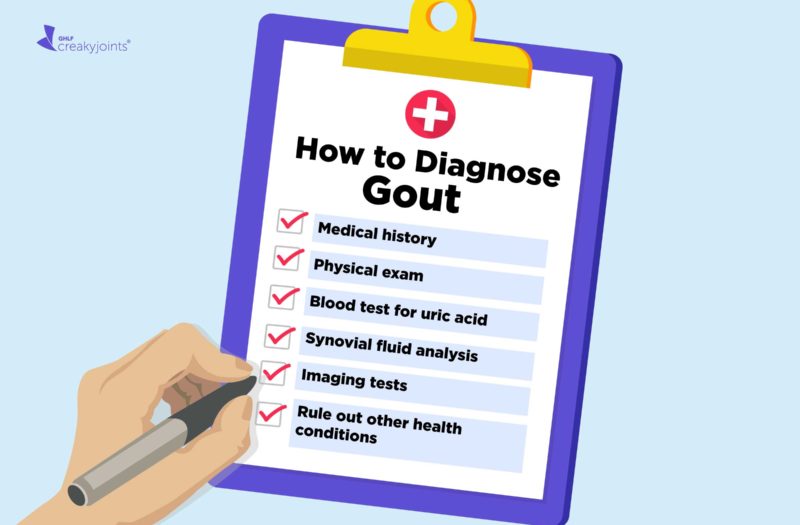
Diagnosing Gout: What to Expect at the Doctor’s Office
If you’re unsure about what’s causing your pain and other symptoms, you’ll likely visit various health care providers, which could include your internist/general practitioner, orthopedist, or podiatrist.
While your GP or internist may be able to diagnose and manage gout, if the diagnosis of gout is not clear, or if you aren’t getting better with initial treatment, you may be referred to a rheumatologist. A rheumatologist is a specialist who treats musculoskeletal disease and systemic autoimmune conditions, including gout.
There is no single, simple test to diagnose gout.
First, your doctor will perform a physical examination to assess your overall health and ask about your history of joint pain and other symptoms that suggest gout, as well as your family history and any pre-existing medical conditions you have or medications you take.
The doctor may check for pain in multiple joints. “Over half of cases of acute gout occur in the big toe for the first time. Then over time, it can spread to other areas, like the middle of the foot, the ankle, knees, hands, the wrists, the elbows, and other joints as well,” says Jonathan Greer, MD, a rheumatologist with Arthritis & Rheumatology Associates of Palm Beach in Florida.
Along with assessing your medical history and your symptoms, your rheumatologist will want to hear about any possible risk factors for gout. Don’t be alarmed if your doctor asks questions about your eating and alcohol consumption habits. These questions will help your doctor identify any lifestyle-related risk factors for gout, such as sugar consumption and heavy, habitual alcohol drinking, so it’s important to be honest.
Risk factors of gout that your doctor may consider:
- Family history of gout
- Obesity (BMI over 30 kg/m2)
- Certain medications, like diuretics (water pills)
- High consumption of foods rich in purines (red meats, organ meats and certain types of seafood (anchovies, herring, sardines, mussels, scallops, trout, haddock, mackerel and tuna)
- Certain chronic health conditions, including congestive heart failure, diabetes, high blood pressure, insulin resistance, kidney disease, and metabolic syndrome
- Heavy, habitual alcohol consumption
Read more here about common gout risk factors and how they may affect you.
Understanding the Diagnostic Criteria for Gout
If you visit your primary care doctor, they will likely use a clinical diagnostic approach (“rule”) that is based on the following variables and scores. If your score is 4 or less, your likelihood of gout is low. If your score is 8 or above, you have a high probability of a gout diagnosis.
- Male sex (2 points)
- Previous patient-reported arthritis flare (2 points)
- Onset of symptoms within one day (0.5 points)
- Joint redness (1 point)
- First metatarsal phalangeal joint (big toe) involvement (2.5 points)
- Hypertension (high blood pressure) or at least one cardiovascular disease (1.5 points)
- Serum (blood) urate level greater than 5.88 mg/dL (3.5 points)
Tests for Diagnosing Gout
Your provider will likely order a series of laboratory tests that help point to gout or rule out other conditions to make a final diagnosis. These tests are often performed during a gout flare, as this is when it’s easiest to find uric acid crystals in the affected joint.
“However, the uric acid level can go down during a flare,” says Dr. Fields, “so in some people it needs to be rechecked when they are not having a flare.”
Synovial fluid analysis
The ideal way to diagnose gout is to draw fluid out of the joint and have the fluid examined for the presence of uric acid crystals under the microscope, with a special attachment called a polarizer, says Dr. Fields.
After using a local anesthetic to numb the soft tissue over the joint, the doctor will insert a needle into the joint space to extract a sample of fluid. The fluid is sent to the lab for analysis and may even be viewed by your doctor. If it’s gout, the synovial fluid analysis will show needle-shaped crystals.
Blood tests
Your doctor will probably use a blood test to help determine whether you have gout. For people with gout, the blood uric acid level is almost always higher than 6 mg/dL, says Dr. Fields. “The higher it is the more gout is suggested as the diagnosis,” he adds.
It’s important to note that people will low urate levels can still have gout — and levels can drop during a flare. In fact, between 12 and 43 percent of people have low to normal uric acid levels during a gout flare, according to UpToDate.
As well, you can have high uric acid levels but not have painful gout symptoms. This is a condition called asymptomatic hyperuricemia.
Imaging Tests
Imaging tests, including X-ray, ultrasound, and computed tomography (CT), can help doctors rule out other health conditions and check for tophi, crystal deposits, and fluid accumulation, which are all characteristic of gout.
X-rays
An x-ray can reveal whether you have any tophi under the skin as well as whether you have any bone erosions due to tophi, which are characteristic of chronic gout. It can also be used to rule out a fracture in your toe or other joint.
Ultrasound or MRI
These can show any crystal deposits, fluid accumulation, or narrowing of the joint space (due to cartilage loss).
DECT Scan
A dual-energy CT scan can be used to distinguish urate crystals (a telltale sign of gout) from calcium crystals (common in another condition known as pseudogout).
Ruling Other Health Conditions
If you are overweight, have sudden, sharp pain in your big toe at night, your blood test reveals high uric acid levels, and you tend to eat a diet rich in meat and seafood and drink alcohol excessively, gout is likely the culprit. But a gout diagnosis is not always that straightforward.
Roughly 25 percent of people with gout don’t even feel pain in the big toe. Instead, the symptoms occur in multiple joints and can mimic other conditions, including:
- Pseudogout
- Septic arthritis
- Bacterial skin infection (cellulitis)
- Stress fracture
- Rheumatoid arthritis
- Psoriatic arthritis
Read more here about common gout misdiagnoses. In these cases, part of the diagnostic process may also involve ruling out these conditions.
Other symptoms and signs that can help your doctor distinguish gout from another form of arthritis include:
- Needle-shaped crystals with sharp edges from a joint fluid analysis
- Lack of symmetry. Gout usually involves just one joint at a time, but even if multiple joints are involved they usually are not symmetrical (i.e. you rarely get both big toes involved at the same time, but rather might get one ankle and one toe).
- Redness over a joint. “This is unusual with rheumatoid arthritis or psoriatic arthritis but common with gout,” he says.
- High intensity of pain and tenderness. The joint hurts to the touch or even from a touch of a sheet.
- Difficulty walking due to the severity of the pain.
- Rapid acceleration of the pain. Gout attacks often reach peak intensity within 24 hours of starting.
After a Gout Diagnosis: Starting Treatment
Luckily, those painful gout attacks are very treatable and manageable if you get a proper diagnosis and start treatment promptly. This will include a variety of medications, to control inflammation and lower your levels of uric acid, along with a few lifestyle modifications to prevent future attacks, including:
- Weight loss. Excess weight can increase uric acid levels and place unwanted pressure on the joints
- Low-purine diet. This means avoiding the “big four”— alcohol, shellfish, red meat, and sugar and high fructose corn syrup.
The most commonly prescribed medication for treating gout is allopurinol (Zyloprim and Aloprim), which helps lower uric acid levels. “It works by blocking the enzymes that transform purines into uric acid,” says Dr. Fields. In people who can’t tolerate allopurinol, or where it isn’t effective, they can be treated with febuxostat (Uloric). Difficult-to-treat gout (also called refractory gout) can be treated with an injectable medication called pegloticase (Krystexxa).
Uric acid-lowering medications are taken regularly to help keep uric acid levels low to prevent crystal accumulation in the joints and elsewhere.
During an acute gout flare, you might need additional medications to reduce inflammation and pain quickly. Treatment for flares includes:
- Anti-inflammatory oral mediations such as colchicine (Mitigare and Colcrys)
- Non-steroidal anti-inflammatories (NSAIDs) such as naproxen (Aleve) or celecoxib (Celebrex)
- Oral steroid such as prednisone or a local steroid injection
While diet changes — such as cutting out high-purine foods, including reducing alcohol intake — can be part of managing gout, many patients make the mistake of over-relying on them to manage their gout. Gout is not a primarily a lifestyle disease; it occurs in people who have a family/genetic predisposition to develop gout and often requires ongoing medication for optimal management.
“The cause of gout is genetics — if you are genetically predisposed to gout you may have a flare set off by certain foods, but if you are not predisposed you may eat them and never feel a gouty pain,” Dr. Fields said in another CreakyJoints report on gout. “It is true that foods such as red meat, shellfish, and alcohol, especially beer, can set off flares of gout, but this happens in people who are genetically susceptible to the condition.”
“Once you start treatment for gout, you are often on it for life,” says Dr. Greer. But here’s the upside: Sticking to your treatment plan also means keeping your gout symptoms out of sight and improving your overall health for years to come.
Track Your Gout Symptoms
Join CreakyJoints’ patient-centered research registry and track symptoms like fatigue and pain. Learn more and sign up here.
Keep Reading
Clinical manifestations and diagnosis of gout. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-gout.
Gout. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Gout.
Gout. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/gout/diagnosis-treatment/drc-20372903.
Gout and Pseudogout Differential Diagnoses. Medscape. https://emedicine.medscape.com/article/329958-differential.
Gout: Diagnosis and Tests. Cleveland Clinic. https://my.clevelandclinic.org/health/diseases/4755-gout/diagnosis-and-tests.
Interview with Jonathan Greer, MD, a rheumatologist with Arthritis & Rheumatology Associates of Palm Beach in Florida
Interview with Theodore R. Fields, MD, a rheumatologist at the Hospital for Special Surgery in New York City
Suresh E. Diagnosis and management of gout. Postgraduate Medical Journal. September 2005. doi: http://dx.doi.org/10.1136/pgmj.2004.030692.
Symptoms and Diagnosis of Gout. Johns Hopkins Arthritis Center. https://www.hopkinsarthritis.org/arthritis-info/gout/clinical-presentation-of-gout.