Ankylosing spondylitis (AS) and psoriatic arthritis (PsA) are both forms of arthritis that cause joint swelling, stiffness, and pain. In AS, these symptoms strike predominantly in the back and sacroiliac joints (where the spine connects with the pelvis), though other joints can be involved. In PsA, symptoms often occur in the hands and feet, and sometimes in other areas, including the knees and back.
Left untreated, both AS and PsA can permanently damage your body. That’s why fast, accurate diagnosis is critical — so your doctor can kickstart treatment to ease pain and prevent long-term issues. The problem is, for a number of reasons, getting the right diagnosis for either condition can often take months or even years. AS and PsA are frequently confused for other diseases, and in some cases, they may even be mistaken for each other.
They are both considered spondyloarthritis, which is an umbrella term for different kinds of arthritis that have some features in common. Spondyloarthritis is considered either axial, which means it mainly affects the spine, or peripheral, which means it mainly affects other joints like the hands, knees, and feet.
While AS is considered “axial” and PsA is considered “peripheral” in reality, symptoms can overlap a lot.
Here’s what you should know about ankylosing spondylitis and psoriatic arthritis — their many similarities, their key differences, and what to do if you suspect you could have either condition.
The Basics of Ankylosing Spondylitis
“Ankylosing spondylitis is a chronic inflammatory disease primarily affecting the spine and sacroiliac joints,” explains Hillary Norton, MD, a rheumatologist at Santa Fe Rheumatology in New Mexico, who has AS herself.
When you have AS, tendons and ligaments along your vertebrae become inflamed, leading to constant pain and stiffness. As time goes on, inflammatory changes in these joints can cause your vertebrae to fuse, limiting your range of motion. AS can also affect other tendons, ligaments, and joints, including those around your knees and shoulders.
AS is part of a disease spectrum known as axial spondyloarthritis (axSpA). In AS, damage from inflammatory arthritis is visible on X-rays. In non-radiographic axial spondyloarthritis (nr-axSpA), which is part of the spectrum, patients have similar symptoms as AS but joint damage is not visible on X-rays.
Experts don’t know what causes AS, but a combination of environment and genes plays a role.
Caucasian, Asian, and Hispanic people are at a higher risk than African American people, but this can often lead to diagnosis delays and misdiagnoses among Africans with AS. As for sex, historically AS has been considered a “man’s disease” but newer research suggests that AS is likely more equally split among men and women. This misconception can lead to diagnosis delays and misdiagnoses among women with AS.
AS typically strikes at a young age compared with other forms of arthritis. Symptoms frequently first affect people in their teens and twenties. Dr. Norton explains that “this kind of pain generally comes on slowly prior to the age of 40.”
AS is associated with many co-occurring diseases, called comorbidities. AS patients have a greater risk of inflammatory bowel disease, heart disease, and stroke. Since AS can involve your ribs, breathing may occasionally become an issue. People with AS who smoke tend to experience more spinal damage than non-smokers.
Read more here of an AS overview.
Common Symptoms of Ankylosing Spondylitis
Lower back pain
“The hallmark symptom is inflammatory back pain,” says Dr. Norton. “Patients often have severe pain in the second half of the night, often causing them to have to get up. Morning stiffness can be significant.” Inflammatory back pain is very different from mechanical back pain due to, say, muscle strains or slipped discs.
The severity of AS pain differs from person to person. At first, the pain is usually dull, constant and slow to develop, building over several weeks and months. It typically involves the lower back and can stay on one side or switch back and forth between sides. (Some people call this “alternating buttock pain.”) As ankylosing spondylitis progresses, the pain can move to the upper back, ribs and neck. The fusing of the vertebrae — and sometimes the ribs — comes later on in the disease course.
While back pain is a signature of AS, patients often experience other symptoms, as well, including:
Enthesitis
“This is inflammation of the tendons and ligaments, such as the Achilles [tendon] or the elbows,” says Dr. Norton. Enthesitis frequently occurs around the heel or sole of the foot and can make standing or walking difficult.
Eye problems
Inflammation of the eye occurs in up to 30 percent of AS patients. This may cause pain, light sensitivity, and blurry vision among other issues, and should be treated by a health care provider.
GI problems
There is a higher risk of developing inflammatory bowel disease among people with AS. If you have chronic GI issues like diarrhea and bloating along with lower back pain, it could be a red flag for AS.
Other symptoms of AS include fatigue and chest pain. Read more here about ankylosing spondylitis symptoms.
The Basics of Psoriatic Arthritis
When people think of psoriatic arthritis, they often immediately associate it with the skin disease psoriasis. Psoriasis is an autoimmune skin condition characterized by scaly red patches that commonly show up on your elbows, knees, and scalp. In about 70 percent of PsA cases, psoriasis appears first, though arthritis symptoms precede psoriasis in about 15 percent of cases and in another 15 percent of cases, the joint and skin symptoms strike at the same time.
Estimates vary, but it’s thought that roughly one in three people with psoriasis will develop psoriatic arthritis over time, according to the Johns Hopkins Arthritis Center.
As with many inflammatory conditions, doctors don’t know what causes psoriatic arthritis, though a combination of environment and genetics are thought to play a role; about four in 10 people with PsA have family with either psoriasis or arthritis. PsA often strikes between the ages 30 and 50 and tends to occur in men and women equally. Caucasian people develop it more often than African or Asian Americans.
Like AS, PsA is also associated with many comorbidities, including inflammatory bowel disease, skin cancer, and depression. Many patients have metabolic syndrome, a group of health problems — including obesity, high blood pressure, and high blood sugar — that raises the risk for heart disease. Heart disease is a common complication among those with PsA.
Common Symptoms of Psoriatic Arthritis
PsA symptoms can vary widely among patients. They can be mild or severe, and can show up abruptly or build slowly but surely over time. People with PsA often have flares, during which symptoms get much worse and then subside.
Joint pain, swelling, and stiffness
People with PsA experience swelling, pain, and stiffness in joints — especially in the fingers and toes. This pain can affect a single joint or many joints and can appear in different parts of the body. Just like with AS, symptoms can especially bad in the morning or after being in the same position for a long time. In PsA, joint pain is less likely to be symmetrical, which is a distinction from rheumatoid arthritis (RA).
Back pain and neck pain
Back and neck symptoms can also occur in people with PsA (which is one of the reasons it can be confused with ankylosing spondylitis).
Psoriasis skin plaques
Since PsA typically occurs in people who have psoriasis, patients often develop scaly patches before arthritis symptoms show up. The severity of symptoms won’t necessarily be the same, however. You may have severe psoriasis with mild PsA or vice versa.
Nail issues
Between 80 and 90 of people with PsA have fingernail or toenail changes. The nails may be pitted or discolored, or they may separate from the skin and crumble completely. It may look like an infection.
Sausage digits
“A hallmark sign of PsA is dactylitis, which is the swelling of an entire finger or toe,” says Dr. Norton. Dactylitis can affect one or more digits and may be painful.
Enthesitis
Enthesitis, or inflammation where tendons and ligaments attach to bone, is also very common in PsA, particularly in the foot.
GI problems
Inflammatory bowel disease can also occur among people with PsA and psoriasis.
Uveitis
As with AS, people with PsA may experience eye inflammation.
Fatigue is also a very common and debilitating symptom in PsA. Read more here about psoriatic arthritis symptoms.
Subtle Differences in Symptoms of Ankylosing Spondylitis and Psoriatic Arthritis
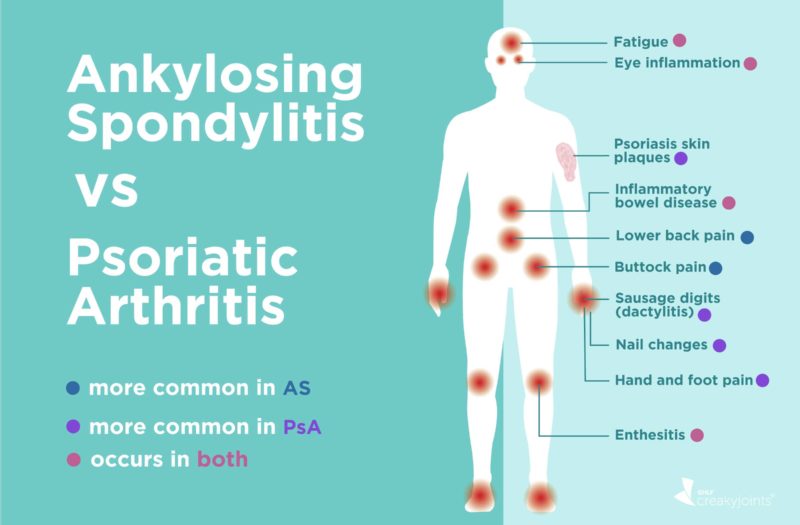
While AS and PsA have many similar symptoms — and are considered to be related diseases —certain differences can help set them apart.
Presence of back pain
AS always affects the spine. “PsA can have axial [spinal] involvement, but the arthritis is primarily in the peripheral joints in most patients,” says Dr. Norton.
Joint pain location
PsA often affects fingers and toes. “When AS has peripheral joint involvement, it is usually the large joints such as the shoulders, hips, and knees,” Dr. Norton explains.
Skin and nail problems
While it’s possible to have PsA and AS at the same time, it’s comparatively rare for AS patients to develop psoriasis or nail issues. They’re much more common in PsA, reported by the vast majority of patients.
Despite these clues, identifying either disease can be complicated and may take a long time. In fact, waiting between seven and 10 years for a diagnosis is normal for people with AS. This is partly because back pain is so common and patients often wait to bring it up with a physician. It’s also due to misdiagnosis; many primary care doctors simply don’t know much about AS, and may mistake it for a different condition like fibromyalgia.
Similarly, PsA can be misdiagnosed for rheumatoid arthritis, osteoarthritis, or gout.
Diagnosing Psoriatic Arthritis vs. Ankylosing Spondylitis
The right diagnosis is vital to treating both PsA and AS, and is best done by a rheumatologist. There is no single test for either condition, so health care providers must rule out other disorders.
To begin, they will take your family and medical history, ask about symptoms and perform a physical exam. They will look for joint pain patterns and locations, as well as other distinguishing symptoms, like skin and nail issues for PsA and the presence of related symptoms, like eye or GI problems.
Lab testing is done to help diagnose AS and PsA. Providers may take blood or joint fluid samples to look for levels of inflammation and discount the possibility of other illnesses, such as gout or rheumatoid arthritis. Patients suspected to have AS or PsA will likely have X-rays to check for damage to the joints. If more information is needed, additional imaging such as MRI or ultrasound can be used. Sometimes skin biopsies are involved.
Many times, especially if AS is suspected, patients will be tested for a genetic marker called HLA-B27. The gene is present in only about 8 percent of the general population but can be found in up to 95 percent of white AS patients and about 50 percent of black AS patients. In PsA, identifying the gene can help predict whether you may have problems with your spine.
“It is an important component of [AS] diagnosis, especially early in disease and in women,” says Dr. Norton. “If HLA-B27 is present along with characteristic symptoms, the specificity of the test greatly increases.”
Read more here about how ankylosing spondylitis is diagnosed and how psoriatic arthritis is diagnosed.
Treatment Options for Ankylosing Spondylitis vs. Psoriatic Arthritis
There is no cure for either AS or PsA. However, in the case of either condition, medication is critical to treat symptoms, protect joints, slow disease progression, and improve quality of life. Your rheumatologist will best determine the best treatment plan for your specific symptoms and health needs, says Dr. Norton.
Some of the treatments for AS and PsA overlap, though certain medications are better for certain symptoms.
For AS patients: Non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil) and naproxen (Aleve) are considered a first-line treatment for ankylosing spondylitis. If these medications don’t adequately relieve symptoms, doctors frequently turn to biologics, which are targeted therapies that act on the immune system to stop inflammation. They are either infused with an IV or injected with a syringe or auto-injector pen.
Different biologics act on different parts of the immune system. In AS, commonly used biologics include those that block the protein tumor necrosis factor (called anti-TNF biologics, or TNF inhibitors) as well as those that block a protein called interleukin-17 (IL-17).
FDA-approved anti-TNF biologics for AS include adalimumab (Humira), certolizumab pegol (Cimzia), etanercept (Enbrel), golimumab (Simponi), and infliximab (Remicade). FDA-approved IL-17 inhibitors for AS include secukinumab (Cosentyx) and ixekizumab (Taltz).
For PsA patients: NSAIDs may also be used to treat more mild cases of PsA, but doctors typically prescribe disease-modifying anti-rheumatic drugs (DMARDs) or biologics to suppress immune system activation and inflammation. DMARDs commonly used to treat PsA include methotrexate, leflunomide (Arava), and sulfasalazine (Azulfidine).
The same TNF inhibitor and IL-17 inhibitor biologics for AS may also be used to treat PsA. There are also additional biologics and targeted therapies for PsA that act in the immune system in other ways. This includes the biologic ustekinumab (Stelara), which blocks IL-23 and IL-12, and abatacept (Orencia), which works on immune system cells called T cells. Oral pills are also available to treat PsA; these include tofacitinib (Xeljanz), which is a type of JAK inhibitor, and apremilast (Otezla), which blocks a protein called PDE4.
PsA patients may also benefit from phototherapy or topical creams to treat skin plaques.
While surgery is not often needed for either AS or PsA, joint repair or replacement can improve mobility and relieve discomfort in people with long-standing disease or more severe cases. In AS, it may occasionally be necessary to straighten the spine.
Healthy Lifestyle Changes
Physical activity is a crucial part of both AS and PsA treatment since it builds strength, prevents stiffness, and helps maintain flexibility and mobility. Speak with a health care provider about a regimen that’s right for you. Exercises like walking, swimming, biking, yoga, and tai chi are popular options. People with AS may especially benefit from practices that focus on posture.
For both AS and PsA, it’s also important to eat right and maintain a healthy weight, which reduces pressure on joints and “can help decrease the inflammatory burden,” says Dr. Norton. For patients who are overweight, losing weight can help relieve symptoms, make medications work more effectively, and reduce the risk of serious comorbidities like heart disease.
Limiting alcohol intake is a good idea, as is quitting smoking. Other treatment options include heat and cold therapies, braces or splints, and relaxation techniques such as deep breathing and mindfulness medication.
Ultimately, whether you have AS or PsA, prompt diagnosis and treatment are key. It’s important to see a rheumatologist to get to the bottom of your symptoms, says Dr. Norton, and most of all, for patients to remember “that they are never alone.”
Not Sure What’s Causing Your Pain?
Check out PainSpot, our pain locator tool. Answer a few simple questions about what hurts and discover possible conditions that could be causing it. Start your PainSpot quiz.
Keep Reading
Ankylosing Spondylitis. Medline Plus. U.S. National Library of Medicine. https://medlineplus.gov/ankylosingspondylitis.html.
Ankylosing Spondylitis. Weill Cornell Brain and Spine Center. https://weillcornellbrainandspine.org/condition/ankylosing-spondylitis/surgery-ankylosing-spondylitis.
Clinical manifestations and diagnosis of psoriatic arthritis. UpToDate. https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-psoriatic-arthritis.
Diagnosis of Psoriatic Arthritis. Spondylitis Association of America. https://www.spondylitis.org/Psoriatic-Arthritis/Diagnosis.
Feld J, et al. Is axial psoriatic arthritis distinct from ankylosing spondylitis with and without concomitant psoriasis? Rheumatology. October 2019. doi: https://doi.org/10.1093/rheumatology/kez457.
Gladman DD, et al. Psoriatic arthritis: epidemiology, clinical features, course, and outcome. Annals of the Rheumatic Diseases. March 2005. Doi: http://dx.doi.org/10.1136/ard.2004.032482.
How Is a Person Affected? Spondylitis Association of America. https://www.spondylitis.org/Possible-Complications.
How does psoriatic arthritis affect the spine? Medical News Today. https://www.medicalnewstoday.com/articles/323320.php.
Interview with Hillary Norton, MD, rheumatologist at Santa Fe Rheumatology in New Mexico
Metabolic Syndrome. Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/metabolic-syndrome/symptoms-causes/syc-20351916.
Overview of Ankylosing Spondylitis. Spondylitis Association of America. https://www.spondylitis.org/Ankylosing-Spondylitis.
Psoriatic Arthritis. American College of Rheumatology. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Psoriatic-Arthritis.
Psoriatic Arthritis. Johns Hopkins Arthritis Center. https://www.hopkinsarthritis.org/arthritis-info/psoriatic-arthritis.
Psoriatic Arthritis. Medline Plus. U.S. National Library of Medicine. https://medlineplus.gov/psoriaticarthritis.html.
Psoriatic Arthritis Symptoms. Spondylitis Association of America. https://www.spondylitis.org/Psoriatic-Arthritis/Symptoms.
Rudwaleit M, et al. Ankylosing Spondylitis and Bowel Disease. Best Practice & Research Clinical Rheumatology. June 2006. doi: http://dx.doi.org/10.1016/j.berh.2006.03.010.
Treatment of Ankylosing Spondylitis and Related Diseases. Spondylitis Association of America. https://www.spondylitis.org/Treatment-Information.
What Is Ankylosing Spondylitis? National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/ankylosing-spondylitis.