If your shoes are feeling tighter than usual or you’re having difficulty or pain opening jars, a type of autoimmune disorder called psoriatic arthritis (PsA) could be to blame. PsA is an inflammatory arthritis linked to psoriasis (a condition causing red, scaly rashes on the skin). It is characterized by pain, stiffness, and swelling in the joints — although these general arthritis symptoms can take on specific characteristics when they are caused by psoriatic arthritis
As with many conditions, early diagnosis and prompt treatment are important. “If you put off seeing the doctor, there are two major concerns with a delayed psoriatic arthritis diagnosis,” says Bharat Kumar, MD, Associate Rheumatology Fellowship Program Director at University of Iowa Health Care and member of the American College of Rheumatology.
First, he explains, disease activity may worsen and cause lasting joint damage. Second, PsA is linked to a higher rate of heart disease, so the sooner you’re diagnosed the quicker you can address cardiovascular factors like high cholesterol and hypertension. “Rheumatologists are eager to see anyone with psoriasis who is also experiencing joint pain,” Dr. Kumar says.
What to Expect at the Doctor’s Office
You may be seeing various health care providers during your journey to figure out what’s causing your symptoms. It’s common for people to see their internist/general practitioner, a dermatologist to treat their psoriasis, or other types of doctors to manage specific areas that are causing pain, such as a podiatrist to treat foot pain. However, if you or any of the health care providers you are currently seeing suspect it could be psoriatic arthritis, ask for a referral to a rheumatologist. These doctors specialize in arthritis and have the training to determine whether your joint symptoms are due to PsA or could be something else.
Psoriatic arthritis can be challenging to diagnose for a number of reasons, including:
1. Having psoriasis isn’t always a reliable clue
Around 70 percent of people with psoriatic arthritis develop psoriasis first, but in the other 30 percent of the time, the arthritis and skin symptoms occur around the same time, people have psoriasis but don’t realize it, or the psoriasis may develop later on after the arthritis-like symptoms show up. Some people can develop psoriatic arthritis without having psoriasis.
2. You can have psoriasis and a different kind of arthritis that is not PsA
People with psoriasis can develop different types of arthritis — including rheumatoid arthritis, gout, osteoarthritis, and reactive arthritis — so diagnosing PsA involves ruling out those other conditions.
“It’s often difficult to say in a first visit whether a patient definitely has psoriatic arthritis or another type of arthritis that just co-exists with psoriasis,” says Dr. Kumar. “PsA can take a long time to diagnose because a patient can delay seeing the doctor, then confirming PsA can require multiple labs and imaging tests.”
The good news is that the diagnosis process for psoriatic arthritis is improving. Whereas PsA wasn’t even recognized as a distinct condition decades ago (it was thought to be rheumatoid arthritis), doctors are now better equipped with improved lab tests and imaging studies that help identify this disease so more patients can find relief.
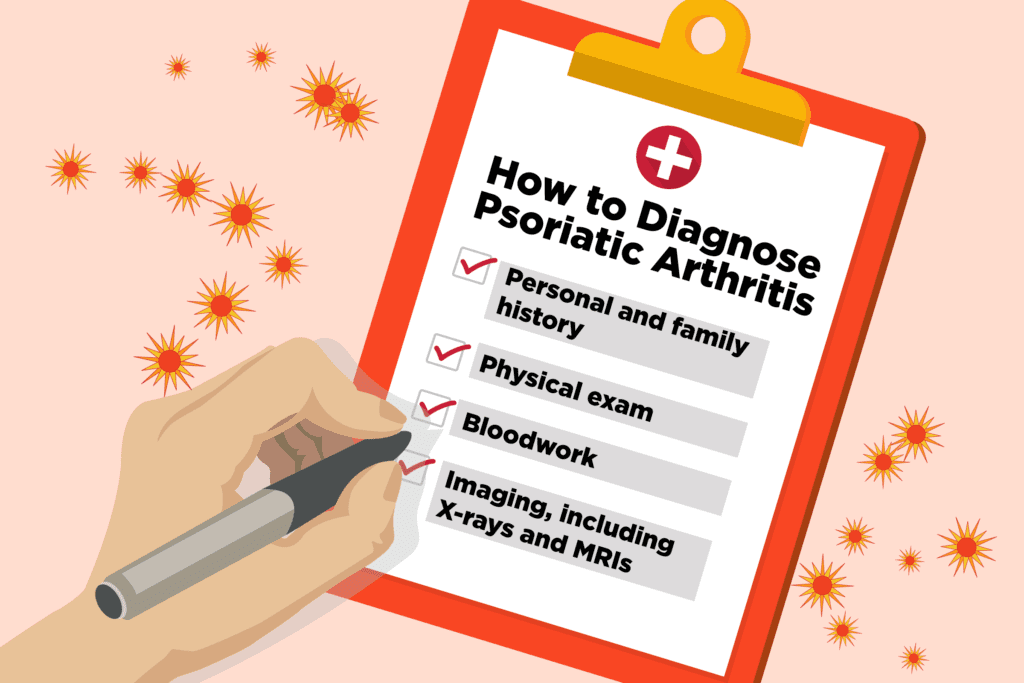
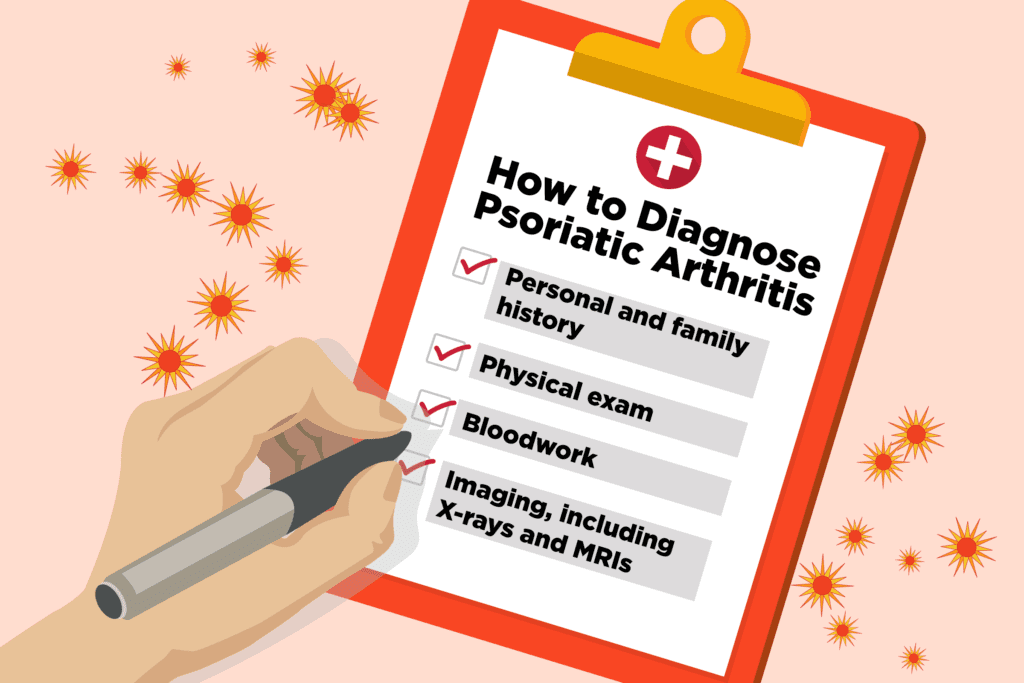
Complete Medical History for Diagnosing Psoriatic Arthritis
Your road to a psoriatic arthritis diagnosis starts with talking to your rheumatologist in order to share symptoms and identify risk factors. While symptoms like joint pain could suggest a number of conditions, in psoriatic arthritis, joint pain often has specific characteristics, including the following:
- Joint pain that gets better with use
- Joint redness and swelling
- Swelling of an entire finger or toe as opposed to just one joint, called dactylitis or “sausage digits”
- Morning stiffness that lasts more than 30 minutes
- Back pain that wakes you up in the second half of the night (back pain at night is also common in ankylosing spondylitis)
- Changes in the nails of your fingers or toes, such as holes, pitting, discoloration or softness, which occurs in 80 to 90 percent of PsA cases
When patients talk about these psoriatic arthritis symptoms, rheumatologists like Dr. Kumar hear a number of common concerns, such as “My shoes don’t fit,” “I feel stiff all over in the mornings,” and “I have trouble opening jars or door knobs.”
Along with listening to your symptoms, your rheumatologist will want to hear about any possible risk factors for psoriatic arthritis. While this condition can affect patients of both genders at a range of ages, the following can increase your risk:
- Having psoriasis
- Having a family history of PsA, psoriasis, or associated conditions, including ankylosing spondylitis, Crohn’s disease, ulcerative colitis, autoimmune uveitis, and reactive arthritis
Physical Exam for Diagnosing Psoriatic Arthritis
The next step in diagnosing psoriatic arthritis is a thorough physical exam, which can involve a number of steps, including the following:
- Looking for signs of psoriasis in usual spots such as elbows and knees, as well as less visible places including the scalp, belly button, intergluteal cleft (“butt crack”), palms of hands, and soles of feet
- Checking the nails of fingers and toes for abnormalities
- Applying pressure to (palpating) joints for tenderness and swelling, as well as looking for redness
- Checking for tendon and ligament issues, including plantar fasciitis and Achilles tendonitis
- Checking for back mobility
- Checking for pain and inflammation along the sacroiliac joints, which is where the spine connects with your pelvis
Laboratory Tests for Diagnosing Psoriatic Arthritis
Your rheumatologist will likely order a series of laboratory tests, the results of which will help check for other conditions or point to psoriatic arthritis. These studies will examine factors such as the following:
- Complete blood count
- Erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP), which are inflammatory markers that might be elevated in PsA but should not be elevated in “wear-and tear” osteoarthritis or arthritis
- Rheumatoid factor (RF) and anti-cyclic citrillunated peptide (CCP), which are antibodies often present in cases of rheumatoid arthritis, but not commonly found in cases of PsA
- Blood urea nitrogen, creatinine, uric acid, and urinalysis
Imaging Studies for Diagnosing Psoriatic Arthritis
In addition to laboratory tests, imaging studies can help your rheumatologist see whether the appearance of your bones and tissues suggests you could have PsA or another condition. Depending on your case and circumstances, your doctor may order one or more of the following tests:
X-ray: A radiograph image of your affected joints — as well as your spine if that appears to be affected — will help your doctor see marginal bone erosions, which means bone being eaten away where it meets a ligament or tendon. This would suggest PsA. Ankylosis (fusing of bones, especially in the spine) may also be seen in very severe PsA. (This is also seen in ankylosing spondylitis.) But a negative X-ray may simply mean the PsA is in an early stage, so additional imaging could be needed.
Ultrasound: A sonogram of the affected joints can help your doctor see disease activity and damage in tendons and ligaments. In cases of psoriatic arthritis, your doctor may see inflammation of tendons and joints (especially where joints meet tendons) or erosions where bone has been eaten away by immune cells.
MRI: Magnetic resonance imaging (MRI) can be especially helpful in allowing your doctor to investigate back pain you might have associated with PsA.
Chances are, if you’re seeing a rheumatologist because you have concerns about having psoriatic arthritis, you’ve already seen quite a few different doctors or health care providers by now. We know this process can be exhausting and exasperating. We are here for you to help make things easier.
Become part of the CreakyJoints community (you can sign up in the upper right corner of our site) and follow us on Facebook and Twitter for ongoing support and education.
Get a more specific list of psoriatic arthritis symptoms here or check out this article on PsA patients’ best advice for coping with the disease.
If you’ve been diagnosed with psoriatic arthritis, download our free guidelines A Patient’s Guide to Living with Psoriatic Arthritis here.





