Psoriasis you can usually spot: the autoimmune disease often causes red patches of skin topped with thick, silvery scales. It occurs when your body’s immune system goes into overdrive, attacking healthy tissue and causing an overproduction of skin cells. But what you can’t see is that same abnormal immune response may also cause inflammation in your joints.
About one-third of people with psoriasis develop psoriatic arthritis (PsA) — a chronic, inflammatory disease of the joints and entheses, or places where tendons and ligaments connect to bone.
Most people with psoriatic arthritis develop psoriasis first, and are later diagnosed with psoriatic arthritis. But joint problems from psoriatic arthritis can sometimes begin before skin signs appear. Or sometimes skin issues are so mild that patients don’t connect psoriasis with joint pain and realize they could have PsA. (That’s what happened to psoriatic arthritis patient Frances Downey.)
Psoriatic arthritis can cause pain, stiffness, and swelling in any joint in your body, from your hands to your back — and often, in your feet. You can read here about common psoriatic arthritis symptoms.
How Psoriatic Arthritis Affects the Feet
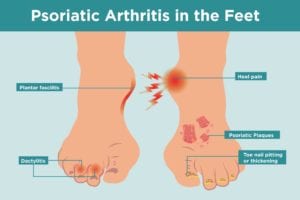
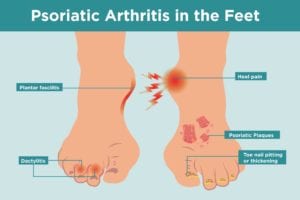
Each foot contains 26 bones and 33 joints that are controlled by a number of muscles, tendons, and ligaments. Inflammation from psoriatic arthritis can occur in any one of those spots, explains Alex Kor, DPM, podiatrist with Witham Health Services in Indiana. Ankle joints can also be affected by psoriatic arthritis, as well as tendons that pass around the ankle and connect the bones with the muscles that move them.
What Does Psoriatic Arthritis in the Feet Feel Like?
When your feet are affected by psoriatic arthritis, you may have pain, tenderness, and swelling in your foot. This occurs when the membranes that line the joints, tendons, and connective tissue in the foot become inflamed. Similar to other forms of inflammatory arthritis, such as rheumatoid arthritis, joints may feel warm to the touch, and stiffness may be worse in the morning or after periods of inactivity.
Symptoms may also flare, then go into periods of remission. Here’s more information about coping with psoriatic arthritis flares.
But unlike with rheumatoid arthritis — where symptoms typically occur in the same joints on both sides of your body (or symmetrically), PsA is usually asymmetrical. “You can have psoriatic arthritis in the ankle joint of one foot and the toe of another,” explains Dr. Kor, who also serves as spokesperson for the American Podiatric Medical Association.
Specific foot problems caused by PsA include:
Sausage toes
Medically speaking, it’s called dactylitis, a condition that refers to swelling of an entire toe (or finger), which gives it a sausage-like appearance. Dactylitis happens when the small joints in the toe, as well as the entheses of the surrounding tendons, become inflamed. An enthesis is the point of insertion of a tendon, ligament, joint capsule, or fascia to bone. Inflammation of the entheses is common in psoriatic arthritis.
Gout — another form of arthritis — also causes pain and swelling in the toes. But with gout, symptoms are sudden, severe, and often target the joint at the base of the big toe. “Psoriatic arthritis can affect multiple joints, and is seen a little more in the third, fourth, and fifth toe joint,” adds Dr. Kor.
Heel pain
In psoriatic arthritis, heel pain stems from inflammation of the Achilles’ tendon, where the tough band of tissue connects your calf muscle to your heel bone. It’s a common spot for inflammation of the entheses when you have PsA.
Pain on the sole of your foot
The plantar fascia is a thick tissue that runs along the bottom of your foot. It connects the toes to the heel bone, and often becomes inflamed when you have psoriatic arthritis. It’s common for people to assume they have only plantar fasciitis, or inflammation of the plantar fascia, when they actually have psoriatic arthritis.
Toe nail changes
Your nails may lift off the nail bed; they may also have pitting (or small indents), discolor, or thicken — similar to a fungal infection. These psoriatic arthritis nail changes occur from abnormalities in the growth of tissue in the nail bed.
How to Keep Your Feet Healthy with Psoriatic Arthritis
Psoriatic arthritis is a chronic condition that can get worse over time. A small percentage of people with PsA develop arthritis mutilans, which is a severe and painful form of the disease that can lead to deformity and disability. Though there’s no cure for psoriatic arthritis, you can take steps to manage symptoms, control inflammation, and protect your joints.
To help keep your feet healthy:
Stick to your PsA treatment plan
Your rheumatologist may prescribe one or more of these medications to manage psoriatic arthritis symptoms and help prevent disease progression:
- Nonsteroidal anti-inflammatory drugs (NSAIDs) to relieve pain and reduce inflammation
- Disease-modifying antirheumatic drugs (DMARDs) to help slow the progression of psoriatic arthritis
- Biologics, which are complex, targeted DMARDs that act on certain immune system pathways
Lose weight if you need to
Maintaining a healthy weight reduces the amount of stress on the joints in your feet, which can help relieve pain and improve your walking gait. Excess body weight can also increase inflammation, and potentially make arthritis symptoms worse. Check out these weight loss tips that are especially helpful when you have arthritis.
Get active
Exercise can help keep joints flexible, boost energy, and burn more calories. Read why exercise is important for PsA patients. Physical activity can also improve vasodilation (or widen blood vessels), which can increase blood flow to the joint to help flush out inflammation, adds Dr. Kor. You don’t have to walk, run, or jump if it hurts, he says.
Choose activities that are less stressful on the joints in your feet, including:
- Elliptical machine exercises
- Stationary biking
- Swimming
- Water aerobics
Stretching exercises, especially ones that are focused on the source of your foot pain, such as the plantar fascia or Achilles’ tendon, can help relieve pain. Here are 20 simple stretches you can do at home. Talk to your doctor or podiatrist about exercises that are safe for you.
Ice after exercise
Cold constricts blood vessels, which decreases blood flow to the joint to help reduce swelling and inflammation, explains Dr. Kor. Grab an ice pack, frozen bag of veggies or stick cubes in a reusable bag — just be sure to use a towel or other barrier between the cold pack and your skin to prevent irritation. Here are more ways to use cold therapy to manage arthritis.
Toss flimsy shoes
And don’t walk barefoot, advises Dr. Kor. Sturdy shoes with good support and a large toe box can help reduce pressure on inflamed areas and swollen toes. Extra cushioning and wide widths may help too. Your podiatrist may also recommend custom orthotics. These shoe inserts are specifically designed to provide more comfort and reduce pressure on bones and tendons in your feet.
Talk to your doctor to determine the best footwear for you. Here are some tips about picking the right shoes when you have arthritis.
Ask about a cortisone shot
These injections can help reduce swelling and inflammation in your heels, the soles of your feet, or a single toe joint. “It’s not a cure-all,” says Dr. Kor. “Used judiciously, cortisone shots can help reduce a flare for some patients.” Learn more about getting cortisone shots to manage arthritis.
Audio Guide: Understanding Psoriatic Arthritis Symptoms
Learn more about the range of symptoms you can experience with psoriatic arthritis. For more audio guides and insights from PsA experts, check out the Psoriatic Arthritis Club podcast.
Interview with Alex Kor, DPM, MS, podiatrist at Witham Health Services in Indiana.





